
Different tools for nailfold capillaroscopic analysis.
Interest in viewing the nail capillaries dates to the late 17th century. Later research by Maurice Raynaud and others in the late 19th and early 20th century first established a direct link between the nailfold capillaries and certain medical conditions. Although underutilized in the past, with the advent of modern digital equipment and the validation of evidence-based methodologies, this is changing. Capillaroscopy is set to become a more important tool for rheumatologists, especially in the evaluation of Raynaud’s phenomenon and systemic sclerosis.1,2
Nail Capillary Anatomy
Capillaroscopy is a method used to examine a patient’s microcirculation and assess pathological changes. It is completely safe and noninvasive. Using some sort of microscopy, the clinician looks through the epidermis of the nailfold to view the capillaries of the distal papillae.3
Ariane Herrick, MD, is professor of rheumatology at the University of Manchester and honorary consultant rheumatologist at Salford Royal NHS Foundation Trust, England. She explains that nailfold anatomy makes it an ideal place to evaluate the microcirculation. In most of the skin, capillaries run perpendicular to the skin surface, and only the tip of the loop is visible.
Dr. Herrick explains, “At the nailfold, capillaries run parallel, rather than perpendicular, to the skin surface, and they can, therefore, be visualized noninvasively when magnified. Capillaries themselves are invisible, but what can be seen is the column of red blood cells within the capillaries.”
This is of interest to rheumatologists in evaluating systemic diseases that involve vascular damage. In some cases, pathogenic changes in capillary morphology may long predate the onset of clinical symptoms. And in patients already diagnosed with a systemic disease, such as systemic sclerosis, the level of capillary damage may reflect internal organ involvement.2
Normal Capillaroscopic Findings
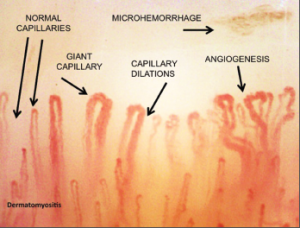
During a capillaroscopic assessment, the practitioner assesses a number of different morphological and functional changes in the capillaries. These include capillary visibility, morphology, diameter, length, distribution and density, microhemorrhages and blood flow. Normal capillary loops display a hairpin “U,” with capillaries running parallel to the skin surface, with no hemorrhages or dilated capillary loops. Capillary density should be 9–12 per mm.1,3,4
Tortuous loops frequently signify pathology, as do abnormally large capillary vessel diameters and decreased capillary density. Microhemorrhages are pathognomonic for systemic sclerosis, especially when seen alongside megacapillaries.1,4
Devices for Nailfold Capillary Exam
A variety of different types of devices can be used to examine the nailfold capillaries. These include dermatoscopes, ophthalmoscopes, traditional microscopes, stereo microscopes or digital video capillaroscopes.2

Dr. Cutolo
Ophthalmoscopes and traditional microscopes are two, low-cost options that are widely available and can be used with minimal training. Dermatoscopes are portable devices at intermediate cost that allow nailfold capillary viewing. Stereo microscopes are the main tools used in national centers due to their ease of use and intermediate cost. But Stereo microscopes can be difficult to use on patients with joint contractures. Dermatoscopes, ophthalmoscopes and traditional microscopes can provide only low magnification, whereas stereo microscopes and video capillaroscopes can provide either low- or high-level magnification.3,5
A video capillaroscope is the most expensive option. It consists of an optical microscope and a digital video camera combined and connected to a computer. The computer can be used to calculate such measurements as the capillary loop diameter and the intercapillary distance.4 It has a handheld probe that can be used for bedside examination or in patients with severe flexion contractures.2 It is available as a portable system, allowing for easy clinical use. Videocapillaroscopy is considered the gold standard for noninvasive examination of the microcirculation. Currently, relatively few rheumatologists have access to this tool, except at large clinical centers, although this may be changing.3
Of note, all of these tools have shown reliability in allowing clinicians to distinguish a normal capillaroscopy exam from the specific changes found in systemic sclerosis.3
Other methods are also available to analyze the microcirculation in detail, including flow Doppler ultrasonography and laser Doppler perfusion imaging.6 However, as Dr. Herrick points out, “Capillaroscopy is the only widely available noninvasive test of the structural microvascular disease, which occurs in systemic sclerosis. Other techniques give an idea of microvascular function (e.g., laser Doppler imaging and, albeit indirectly, infrared thermography). However, these are not a substitute for capillaroscopy but rather provide complementary information.”
Assessment of Raynaud’s Syndrome
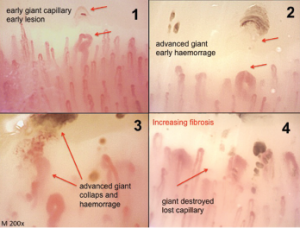
Classical morphological changes of the microvessels (irreversible and pathological) that identify different steps of the sclerodermic microangiopathy (magnification 200X).
Currently, capillaroscopy’s main application is in the assessment of patients with Raynaud’s phenomenon. Raynaud’s phenomenon is characterized by paroxysmal reversible episodes of vasospasm in the peripheral small vessels of the fingers or toes. In primary Raynaud’s phenomenon (about 80% of patients), this occurs without the presence of underlying disease. However, secondary Raynaud’s phenomenon is associated with other medical conditions, most commonly connective tissue disease. In secondary Raynaud’s phenomenon, unlike primary Raynaud’s phenomenon, patients have structural vascular damage that can be viewed via nailfold-viewing methods.7
The connective tissue disease most frequently associated with Raynaud’s phenomenon is systemic sclerosis, followed by mixed connective tissue disease, but it’s also sometimes seen in lupus, rheumatoid arthritis, Sjögren’s syndrome and others. It is also important for clinicians to recognize that Raynaud’s phenomenon sometimes accompanies other disease conditions, such as vasculitis, hematological disorders and malignancy.7
It’s extremely important to differentiate patients with primary Raynaud’s phenomenon from those with secondary Raynaud’s phenomenon. Dr. Herrick explains, “Capillaroscopy can allow early diagnosis of systemic sclerosis, because Raynaud’s phenomenon is the most common presenting feature of systemic sclerosis. Normal nailfold capillaries are reassuring. Conversely, definitely abnormal capillaries point to an underlying systemic sclerosis-spectrum disorder. Sometimes the test is equivocal, and sometimes the capillaries cannot be easily seen. If diagnostic uncertainty remains, then consideration should be given to repeating the capillaroscopy in six to 12 months.”

Raynaud’s syndrome.
Along with capillaroscopy, clinical history and exam, clinicians should run basic ANA and ESR tests to rule out the possibility of secondary Raynaud’s phenomenon. If any clinical suspicion remains, physicians should request additional laboratory assessments for connective tissue disease.7
The problem for the clinician is that some patients presenting with primary Raynaud’s phenomenon will eventually transition to secondary Raynaud’s phenomenon. A meta-analysis indicated 20% of patients initially diagnosed with primary Raynaud’s phenomenon later transitioned to secondary Raynaud’s phenomenon over a follow-up period of 10 years.8
Maurizio Cutolo, MD, is professor of rheumatology and director of the research laboratories and clinical academic unit of rheumatology at the University Medical School of Genova, Italy. Dr. Cutolo advocates nailfold viewing of these primary Raynaud’s phenomenon patients every six months. “The nailfold videocapillaroscopic analysis of patients with primary Raynaud’s phenomenon is the most practical, cheap and reliable system to very early detect the development of a connective tissue disease like systemic sclerosis, even before the appearance of specific autoantibodies in the serum.” Other clinicians have recommended such assessments every 12–24 months in patients with primary Raynaud’s phenomenon.2
Patients who have symptoms of primary Raynaud’s phenomenon and who also have systemic sclerosis specific changes on capillaroscopy are very likely to transition to definitive systemic sclerosis (SSc). SSc-specific antibodies (anti-centromere protein B, anti-topoisomerase I, anti-Th/To, or anti-RNA polymerase III) can also be helpful in establishing prognosis. Patients who do not have any SSc-specific autoantibodies or abnormal nailfold capillaroscopy findings are extremely unlikely to ever develop secondary Raynaud’s phenomenon. In contrast, one study found that 80% of patients with both abnormalities developed systemic sclerosis over 20 years of follow-up.9
Clinicians can also utilize prognostic indices based on capillaroscopy findings to assess the probability of progression to SSc. Using the Prognostic Index for Nailfold Capillaroscopic Examination (PRINCE), clinicians can use specific findings to estimate the five-year probability of secondary Raynaud’s phenomenon developing in patients with isolated Raynaud’s phenomenon. The presence of giant capillary loops, microhemorrhages and reduced capillary number seem to be the characteristics with the most predictive role.10
Systemic Sclerosis
Identifying patients in the very beginning stages of SSc is important, because early use of vascular remodeling drugs may alter the disease course.8 Currently, no treatment for SSc has been clinically proven to halt the disease progression in people with clinically recognizable disease, but available treatments may make a difference if started earlier, before irreversible damage has occurred.3
In 2000, Dr. Cutolo and colleagues first categorized the morphological patterns that can be observed in SSc.11 These can be used to help stage the disease and evaluate drug therapy. It’s important to note the extent of microvascular damage correlates with the severity of skin, heart and lung involvement.12
Dr. Cutolo notes, “Distinct morphological patterns on nailfold videocapillaroscopy and a gradual increase in severity of microvascular abnormalities (quantifiable and scored) are observed during clinical progression of systemic sclerosis and seem to reflect the evolution of the disease process.” The changes reflect the pathophysiological changes characteristic of the disease, with hypoxia over time leading to capillary modification and neo-angiogenesis directed by growth factors in a profibrotic environment.5
An early pattern is characterized by the appearance of several dilated capillaries, some bleeding, but without loss of capillary loops. This early pattern can be often be detected many years before the full clinical manifestations of SSc become apparent.2
In somewhat more advanced disease, an active pattern appears, displaying frequent bleeding megacapillaries, moderate loss of capillaries, moderate disorganization of the capillary architecture and rare or absent branching capillaries.3
Even more advanced scleroderma is characterized by a late pattern, which shows severe capillary loss, neovascularization by megacapillaries and massive avascular areas. This late pattern is more frequent in patients who have active disease and moderate to severe skin or visceral involvement.11
In general practice, clinicians generally categorize these patterns qualitatively based on pattern recognition. However, there are semi-quantitative methods and quantitative methods that can be used to assess certain characteristics of the capillaries using manual or automatic methods. Researchers have also used scoring systems to assess the risk of digital ulceration as a complication. Other studies have looked at the association between capillaroscopic findings and the onset of interstitial lung disease, pulmonary artery hypertension, cardiac involvement, skin involvement and death.3,12
Pathogenic changes in capillary morphology may long predate the onset of clinical symptoms. And in patients already diagnosed with a systemic disease, such as systemic sclerosis, the level of capillary damage may reflect internal organ involvement.
Evaluation of Treatment Response
Microhemorrhages represent the death of the giant capillaries. Their disappearance from the microvessel array, with consequent loss of capillaries, is followed in advanced stages by angiogenesis and the formation of new, abnormal vessels.
Researchers have also used semi-quantitative and quantitative scoring systems in nailfold capillaroscopy to evaluate treatment response in systemic sclerosis. This remains a promising area of research development.
Dr. Cutolo and colleagues evaluated the effect of the vasodilator iloprost compared to iloprost taken with bosentan (an endothelin receptor antagonist). They found that the group taking both iloprost and bosentan had increases in capillary number as assessed by nailfold capillaroscopy at two to three years follow-up.13 Later studies have shown that the drug combination exerts a remodeling effect on the microvasculature, decreasing the likelihood of digital ulceration and helping to stabilize lung function.14
Capillaroscopy may also be of benefit in evaluating certain patients with interstitial lung disease. Such lung disease is commonly found in SSc and related diseases, but it can also be found in other situations, such as from environmental factors or infection. Patients with interstitial lung disease and capillaroscopic findings indicative of systemic sclerosis are likely to soon develop the full feature of systemic sclerosis or a closely associated disease.2
Similarly, capillaroscopy can provide an initial screening technique for interstitial lung disease in patients with mixed connective tissue disease or scleromyositis. The technique can also sometimes be beneficial in helping to distinguish dermatomyositis from polymyositis. In the former, severe capillary abnormalities are common, similar to the scleroderma pattern; in polymyositis, any abnormalities tend to be mild.2
Researchers have extensively examined nailfold capillary characteristics in many other rheumatic diseases, but for the most part have not found repeatable patterns of significance. Patients with lupus, antiphospholipid syndrome, Sjögren’s syndrome or other connective tissue diseases may also show nonspecific abnormalities. It should be noted that nonspecific abnormalities on capillaroscopy can also be found as sequelae from other medical conditions, such as advanced diabetes or hypertension.2
Barriers to Use
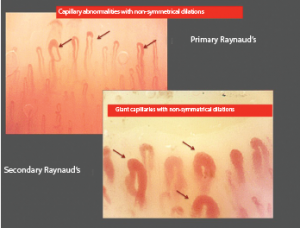
Early structural changes in a patient with Raynaud’s phenomenon (left picture) that should identify very early alterations of the microvessels (dilations under 50 micrometers). The subsequent early morphological changes that identify the secondary associated systemic sclerosis are the presence of symmetrical dilations over 50 micrometers, called giant capillaries (right picture).
Capillaroscopy has been relatively slow to be accepted and widely used as a tool, but that is changing. Dr. Cutolo explains that the slow adoption was mainly due to the absence of clear validation and scoring and classification of capillaroscopic patterns. It has become more adopted as researchers have addressed these concerns and as the technique has demonstrated its value in early differential diagnosis and prediction for clinical complications in SSc.
In 2013, the ACR and EULAR published a new system of classification for SSc. For the first time, abnormal nailfold capillaries were included as part of the scoring.15 Dr. Herrick believes this change has provided a huge incentive for rheumatologists to start using the technique. “This is because abnormal nailfold capillaries score 2 out of the 9 points required to fulfill the criteria. In consequence, this behooves anyone whose clinical practice involves diagnosing systemic sclerosis-spectrum disorders to be familiar with the technique.”
The new classification criteria have increased sensitivity compared with earlier scoring systems, increasing the number of early and mild cases of SSc, which can be successfully recognized.16
Dr. Herrick views lack of familiarity with the technique as a major barrier making nailfold capillaroscopy an underutilized method in clinical practice. However, she explains that this is changing because of increasing numbers of publications in rheumatology journals relating to nailfold capillaroscopy, posters and oral presentations on capillaroscopy at all the main rheumatology meetings and training courses on capillaroscopy.

Dr. Herrick
Cost is another perceived barrier to use. “High-magnification videocapillaroscopy systems (which are considered the gold standard) can be costly, although these are now relatively less expensive than previously with some videocapillaroscopy systems being in the order of £8,000–10,000 [roughly $10,000–13,000 USD],” Dr. Herrick notes. “However, for routine practice, other options are much less expensive. Definite abnormalities can often be seen using simple handheld systems, such as a dermatoscope and low-cost USB microscope.”
What Technique to Use?
A rheumatologist looking to incorporate a method of viewing nailfold capillaries may wonder which method makes the most sense. The answer probably depends on the needs of the specific practitioner.
Ongoing studies are comparing videocapillaroscopy (high magnification, usually 200X) with dermoscopy (low magnification, usually approximately 10X).6 Dr. Herrick notes, “The evidence available so far suggests that dermoscopy is likely to be slightly less sensitive (but more specific) than videocapillaroscopy in detecting scleroderma-pattern abnormalities.”
Dermatoscopes provide an easy method of evaluation for nail capillary pathology, but rheumatologists do not use them as commonly. This may be because rheumatologists are not as familiar with dermatoscopes and their diagnostic abilities in this setting.6
“In my opinion, a dermatoscope or low-cost USB microscope is likely to be the best option for a general rheumatologist, because these allow a very rapid look at the nailfolds in a busy outpatient clinic,” recommends Dr. Herrick.
However, she cautions that subtle abnormalities can be missed with this method. “For someone who is referred a large number of patients with systemic sclerosis, then a videocapillaroscopy system has the advantage of giving a more detailed view of the capillaries and allows measurement of capillary density.” She also notes that a videocapillaroscopy system is the best option for clinical researchers, who often wish to quantify abnormality, something not currently possible with low-magnification systems.
When choosing which type of equipment to purchase, rheumatologists should also think about whether image storing is important for their use. Dr. Herrick notes, “Most commercially available videocapillaroscopy systems allow for easy storage of images, which can then be uploaded onto the patient’s electronic record.” Digitally stored images can also easily be sent via the Internet for telediagnosis and teleconsultation.
Training
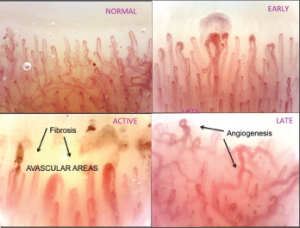
The three validated capillaroscopic qualitative patterns (early, active and late) that characterize the progressive damage of the microvasculature in systemic sclerosis. The concomitant count of the capillaries (within 1 linear mm inside the picture) allows us to quantify and score the progression of the disease. Prediction of clinical complications and prognostic evaluations are supported by the changes in capillary number.
Attaining proficiency in assessing nailfold capillaries via videocapillaroscopy does take more time than some other methods.5 However, Dr. Herrick notes, “It does not take long to become reasonably competent in acquiring and analyzing images, and after a one- to two-day training course, most clinicians will feel reasonably confident in any of the techniques. As with most methodologies, to stay confident and competent, it is necessary to use capillaroscopy regularly.”
Since 2004, EULAR has offered a three-day training course in capillaroscopy every other year. The next scheduled course will be September 2018 in Genova, Italy. For the past six years, the ACR/ARHP Annual Meeting has also offered a workshop on practical capillaroscopy. Dr. Herrick notes that other countries and regions are also running training courses. The Atlas of Capillaroscopy in Rheumatic Diseases is another helpful training tool.
Dr. Cutolo says nailfold capillaroscopy has been slower to be adopted by U.S. practitioners, perhaps partly because it has only more recently begun to be discussed at clinical conferences there. Partly to address this need, Dr. Cutolo and colleagues developed an educational curriculum to teach rheumatology fellows the skills needed to assess nailfold capillaries at the Hospital for Special Surgery in New York. Specifically, the study aimed to teach rheumatology fellows how to use dermoscopy as a tool to diagnose systemic sclerosis while in the clinic. In a one-day course, residents increased their skills in recognizing capillaroscopy abnormalities. Currently, most American rheumatology fellowship programs do not have standardized training in nailfold capillaroscopy.17
Promising Research Avenues
In future research, Dr. Herrick believes we will learn more about how capillaroscopy can help predict disease course in SSc. Other promising research is studying capillaroscopy to assess treatment response and disease process. She explains, “With this aim in mind, at the University of Manchester, we are researching automated analysis of capillaroscopy images using a machine learning approach.”
Hopefully, nailfold capillaroscopy will allow researchers to assess whether early interventions with available vascular remodeling drugs may be able to help prevent disease progression in early SSc.8 As new drugs become available, videocapillaroscopy in particular may provide a powerful research tool to help assess treatment response at all stages of disease for this illness that is currently so difficult to treat.
Ruth Jessen Hickman, MD, is a graduate of the Indiana University School of Medicine. She is a freelance medical and science writer living in Bloomington, Ind.
References
- Criveanu C, Ciurea PL, Musetescu AE, et al. Capillaroscopy—a valuable tool for the assessment of vascular impairment in systemic sclerosis. Romanian Journal of Rheumatology. 2016;25(3):112–116.
- Chojnowski MM, Felis-Giemza A, Olesińska M. Capillaroscopy—a role in modern rheumatology. Reumatologia. 2016;54(2):67–72. doi:10.5114/reum.2016.60215.
- Smith V, Thevissen K, Trombetta AC, et al. Nailfold capillaroscopy and clinical applications in systemic sclerosis. Microcirculation. 2016 Jul;23(5):364–372. doi:10.1111/micc.12281.
- Sood I, Dadhaniya N, Upadhyaya SK, et al. Nailfold capillaroscopy—an underutilised investigation in rheumatology. Apollo Medicine. 2017;14:21–26.
- Roldán LMC, Franco CJV, Navas MAM, et al. Capillaroscopy in systemic sclerosis: A narrative literature review. Rev Colmb Reumatol. 2016;23(4):250–258.
- Dogan S, Akdogan A, Atakan N. Nailfold capillaroscopy in systemic sclerosis: Is there any difference between videocapillaroscopy and dermatoscopy? Skin Res Technol. 2013 Nov;19(4):446–449. doi:10.1111/srt.12067.
- Linnemann B, Erbe M. Raynaud’s phenomenon—assessment and differential diagnoses. Vasa. 2015 May;44(3):166–177. doi:10.1024/0301-1526/a000426.
- Herrick AL, Cutolo M. Clinical implications from capillaroscopic analysis in patients with Raynaud’s phenomenon and systemic sclerosis. Arthritis Rheum. 2010 Sep;62(9):2595–2604. doi:10.1002/art.27543.
- Koenig M, Joyal F, Fritzler MJ, et al. Autoantibodies and microvascular damage are independent predictive factors for the progression of Raynaud’s phenomenon to systemic sclerosis: A twenty-year prospective study of 586 patients, with validation of proposed criteria for early systemic sclerosis. Arthritis Rheum. 2008 Dec;58(12):3902–3912.
- Ingegnoli F, Boracchi P, Gualtierotti R, et al. Prognostic model based on nailfold capillaroscopy for identifying Raynaud’s phenomenon patients at high risk for the development of a scleroderma spectrum disorder: PRINCE (prognostic index for nailfold capillaroscopic examination). Arthritis Rheum. 2008 Jul;58(7):2174–2182. doi:10.1002/art.23555.
- Cutolo M, Sulli A, Pizzorni C, Accardo S. Nailfold videocapillaroscopy assessment of microvascular damage in systemic sclerosis. J Rheumatol. 2000 Jan;27(1):155–160.
- Ingegnoli F, Smith V, Sulli A, Cutolo M. Capillaroscopy in routine diagnostics: Potentials and limitations. Curr Rheumatol Rev. 2017 Jun 14. doi:10.2174/1573397113666170615084229.
- Cutolo M, Ruaro B, Pizzorni C, et al. Longterm treatment with endothelin receptor antagonist bosentan and iloprost improves fingertip blood perfusion in systemic sclerosis. J Rheumatol. 2014 May;41(5):881–886.
- Trombetta AC, Pizzorni C, Ruaro B, et al. Effects of longterm treatment with bosentan and iloprost on nailfold absolute capillary number, fingertip blood perfusion, and clinical status in systemic sclerosis. J Rheumatol. 2016 Nov;43(11):2033–2041.
- van den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: An American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Ann Rheum Dis. 2013 Nov;72(11):1747–1755. doi:10.1136/annrheumdis-2013-204424.
- Jordan S, Maurer B, Toniolo M, et al. Performance of the new ACR/EULAR classification criteria for systemic sclerosis in clinical practice. Rheumatology (Oxford). 2015 Aug;54(8):1454–1458. doi:10.1093/rheumatology/keu530.
- Hatzis C, Lerner D, Paget S, et al. Integration of capillary microscopy and dermoscopy into the rheumatology fellow curriculum. Clin Exp Rheumatol. 2017 Feb 10. [Epub ahead of print]

