 Harvard researchers have created a living, human-gut-on-a-chip that can be used to study the role of the microbiome in gut pathophysiology. The microdevice makes it possible to dissect disease mechanisms in a controlled manner and represents a marked advance over current in vitro systems and animal models. Hyun Jung Kim, PhD, now an assistant professor at the University of Texas in Austin, and colleagues published a description of their human gut-on-a-chip on Dec. 9, 2015, in the Proceedings of the National Academy of Sciences.
Harvard researchers have created a living, human-gut-on-a-chip that can be used to study the role of the microbiome in gut pathophysiology. The microdevice makes it possible to dissect disease mechanisms in a controlled manner and represents a marked advance over current in vitro systems and animal models. Hyun Jung Kim, PhD, now an assistant professor at the University of Texas in Austin, and colleagues published a description of their human gut-on-a-chip on Dec. 9, 2015, in the Proceedings of the National Academy of Sciences.
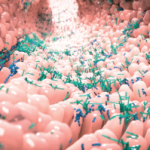
The chip includes Caco-2 intestinal epithelial cells that were originally isolated from a human colorectal tumor in a stable ecosystem with gut bacteria and immune cells. The gut-on-a-chip should provide insights into inflammatory bowel disease (IBD) and ileus. It can be used to define potential therapeutic targets for these conditions and test drug candidates. The gut-on-a-chip should also facilitate evaluation of the growth and treatment of pathogenic bacteria, including the role of physiological mechanical deformation in the induction of small intestinal bacterial overgrowth (SIBO).
The human gut microbiome is believed to play a critical role in the control of gut homeostasis, immune modulation and pathology. Experts believe that chronic intestinal inflammation results from the recruitment of peripheral blood mononuclear cells (PBMCs) into the lamina propria. The chip makes it possible to study this process more closely. In their paper, the researchers describe their investigation of SIBO, the resulting lipopolysaccharides (LPS) and inflammation.
LPS is found in the outer membrane of gram-negative bacteria. It acts as an endotoxin in mammals and promotes the secretion of pro-inflammatory cytokines, nitric oxide and eicosanoids. Although LPS is often present in the human intestine, the levels are generally considered harmless, possibly due to the fact that LPS can, at least partially, be inactivated by mammalian cell-derived acyloxyacyl hydrolase. The gut-on-a-chip allowed the scientists to investigate this process more closely.
“Using this microdevice, we also discovered that immune cells must be present along with LPS or nonpathogenic bacteria to induce production of a key set of proinflammatory cytokines (IL-8, IL-6, IL-1β and TNF-α) that act together to produce villus injury and intestinal barrier disruption,” write the authors in their discussion. “However, although our results confirm that IL-6, IL-1β and TNF-α may contribute to development of intestinal inflammatory disease as suggested in the past based on in vivo studies, our ability to manipulate these factors independently revealed that these cytokines must act in the presence of high levels of IL-8 to exert these disease-promoting effects. This novel result would be difficult to detect using animal models.”