IgA vasculitis is poorly understood, but it mainly affects the skin, the joints, the gastrointestinal tract and the kidneys.
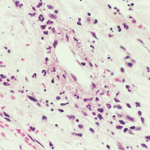
John Watney / Science Source.com
CHICAGO—Diagnosing and treating IgA vasculitis—leukocytoclastic vasculitis involving deposits of IgA1 deposits on the walls of small vessels—is rife with uncertainties, outright unknowns and treatment challenges, an expert on the disease said at the ACR’s 2016 State-of-the-Art Clinical Symposium.
Alexandra Villa-Forte, MD, MPH, staff physician at Cleveland Clinic’s Center for Vasculitis Care and Research, said IgA vasculitis—which used to be known as Henoch-Schönlein purpura and mainly affects children—is poorly understood. It mainly affects the skin, the joints, the gastrointestinal tract and the kidneys, but it can arise in nearly any organ, she said.
Incidence
It appears that there could be a strong environmental component to the disease. In children, peak incidence comes in fall and winter, and the disease is often seen following respiratory infections.
The annual incidence in children is 3–26 cases per 100,000 children—quite a wide range—and is anywhere from two to 33 times more common in children than adults. About 90% of cases are believed to occur in children younger than 10, Dr. Villa-Forte said.
“The problems with defining the disease make it hard to know the incidence of the disease,” she said.
Criteria
Efforts to write criteria to describe it have been only somewhat successful, she said. For example, the 1990 ACR criteria said that someone had the disease if they exhibited two of these four: 20 years old or younger; palpable purpura; acute abdominal pain; or biopsy showing granulocytes in the walls of small arterioles or venules. But because most of those getting the disease are children, they already meet one of the criteria, and that can lead to excessive sensitivity, Dr. Villa-Forte said.
Under the EULAR criteria for children—not adapted for adults—IgA vasculitis is considered to be present with purpura and either abdominal pain, IgA finding on histopathology, arthritis or arthralgia, or renal involvement.
If someone exhibits the “classic triad” for the disease—purpura, arthralgia and abdominal pain—suspicion is raised, but those are not always present, Dr. Villa‑Forte said.
“If you don’t have a high suspicion for the disease clinically, it’s hard to make this diagnosis,” she said.
Cutaneous purpura is universal in the disease, with arthralgias in about two-thirds of the cases, but arthritis is rare. GI involvement is also seen about two-thirds of the time, and intussusception, infarction and perforation are possible.