LONDON—Despite the detailed terminology for describing vasculitis established by the Chapel Hill Consensus (CHC) in 2012, the field badly needs better classification and diagnostic criteria for the group of diseases, an expert said in a presentation at the Annual Congress of the European League Against Rheumatism (EULAR 2016).
It’s a topic that is now being rigorously studied, with results likely coming in the next year or two, said Cees Kallenberg, MD, PhD, the former head of the department of rheumatology and immunology at the University Medical Center Groningen in The Netherlands, in a talk on the latest in the field.
The Vocabulary of Vasculitis
The umbrella term vasculitis—inflammation of the blood vessels that can affect a wide variety of organs—covers a broad range of diseases and syndromes based on vessel size, organ involvement and the likely causes. The groupings in the nomenclature from the CHC include large-, medium- and small-vessel vasculitis; single-organ vasculitis, such as cutaneous arteritis; primary central nervous system vasculitis; and those associated with probable etiologies, such as vasculitis associated with hepatitis B and drug-associated immune-complex vasculitis.
The problem with this vocabulary is that it “does not give diagnostic or even classification criteria,” Dr. Kallenberg said.
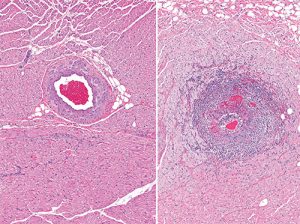
Severe inflammation of the artery (arteritis) (right) in the myocardium. For comparison, a normal healthy artery is shown on the left.
He gave an example from the 1990 American College of Rheumatology classification criteria to convey the need for improvements. The criteria for granulomatosis with polyangiitis (GPA) are nasal or oral inflammation; abnormal chest X-ray; microhematuria; and granulomatous inflammation on biopsy. If someone already has a diagnosis of vasculitis on histology and two of those four are present, a disease can be classified as GPA. But these criteria cannot be used as a diagnostic guide, Dr. Kallenberg said.
“If we use [these] criteria as diagnostic criteria, you must [diagnose] every patient with purulent nasal discharge and microhematuria [with] GPA, which is certainly not right,” he said. “So we definitely need better diagnostic and classification criteria.”
A large, multi-center, international prospective study—the DCVAS study—is underway to design and validate classification and diagnostic criteria, he noted.
ANCA+/-
Another big issue facing the field is whether ANCA-associated and ANCA-negative eosinophilic granulomatosis with polyangiitis (EGPA) should be considered as two different diseases, given that so many differences exist between the two. For example, the ANCA-associated form is typically a small-vessel vasculitis, while ANCA-negative is marked by tissue infiltration with eosinophils.