A 66-year-old male patient presents to the office with right knee pain. He was in the office two weeks prior for a follow-up visit of his primary osteoarthritis. He received an injection of hyaluronate sodium in his right knee four months before and states that his knee felt like new. He states that everything was fine until he decided to lay some tiles. He exacerbated the knee pain by getting up and down multiple times and kneeling for long periods of time. There is swelling in his right knee, and pain is sharp and piercing with a pain level of 8 out of 10.
Drug allergy: No known drug allergies
Current medications:
- Silodosin 8 mg capsule, once daily;
- Verapamil hydrochloride 120 mg tablet, once daily;
- Folic acid 400 mcg tablet, oral;
- Vitamin B-12 250 mcg tablet, oral; and
- Glucosamine 1,500 complex, oral.
Past medical, family, social histories have not changed since last taken on Jan. 4, 2016.
Vital signs: His weight is 280 lbs., height 5’ 8”, blood pressure is 130/88, and his BMI is 44.
The patient is in a friendly and pleasant mood. His knee shows bony hypertrophy, moderate effusion and warmth. He has pain with range of motion and tender palpation.
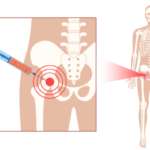
The patient was prepped for injection, and the risks were discussed. Using sterile technique, with a 22-gauge needle, 2 cc of lidocaine and 80 mg of methylprednisolone acetate were used for the injection; 47 cc of clear amber fluid was aspirated from the right knee. The injection was performed via ultrasound guidance because the patient is obese. Synovial fluid analysis with polarized microscopy did not reveal birefringent crystals:
- Inject depo 80 mg;
- Inject lidocaine HCL 2 cc; and
- Synovial fluid crystal analysis.
A return visit is scheduled for six weeks.