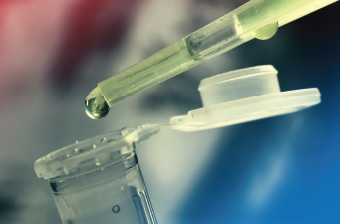
Stem cells in a fluid are being transferred for study.
CI Photos/shutterstock.com
Rheumatologists now have another treatment option to offer their patients with one of, if not the most, difficult autoimmune diseases to treat. New data add to the growing evidence of the safety and benefit of stem cell transplantation for patients with systemic sclerosis with internal organ involvement.
New results of the Scleroderma: Cyclophosphamide or Transplantation (SCOT) trial show that patients with systemic sclerosis with lung involvement who underwent myeloablative autologous hematopoietic stem cell transplantation (HSCT) had superior long-term outcomes compared with patients treated with monthly intravenous cyclophosphamide (CYC).
Reporting on the results of the trial at the 2016 ACR/ARHP Annual Meeting, Keith Sullivan, MD, James B. Wyngaarden Professor of Medicine in the Division of Cellular Therapy, Duke University Medical Center, Durham, N.C., says the results suggest it’s time to consider this treatment approach for select patients with systemic sclerosis with early, severe internal organ involvement.1
“Our job is to fully inform the patient and caregiver of the results of randomized clinical trials and the usefulness of the procedure,” he says, emphasizing that rheumatologists now have a treatment option for this difficult and often fatal disease that patients should know about.
“I’m not trying to oversell this,” he says, “I am trying to have colleagues see things through patients’ eyes, because if the patient never gets referred for a consultation with a transplant physician, this treatment will never be an option for them.”
What the Data Show
Results of the multicenter SCOT trial (currently in peer review for publication) support and expand the evidence for the superiority of stem cell transplantation compared with pulse CYC for select patients with systemic sclerosis, previously reported in the Autologous Stem Cell Transplantation International Scleroderma (ASTIS) trial, and to a more limited degree (because of shorter follow-up of a smaller patient cohort), in the American Scleroderma Stem Cell vs. Immune Suppression Trial (ASSIST).2
In the SCOT trial (sponsored by the National Institutes of Health, National Institute of Allergy and Infectious Diseases), 75 patients with diffuse cutaneous systemic sclerosis and progressive lung or renal involvement were randomized to CYC (750 mg/m2/month) infused over one year (n=39) or myeloablative HSCT (n=36). Unlike the ASTIS and ASSIST trials in which patients were given nonmyeloablative high-dose CYC for both preparative conditioning and stem cell mobilization, the SCOT trial used a lower dose of pre-transplant CYC and employed total body irradiation conditioning to eliminate all autoreactive immune cells prior to stem cell rescue.