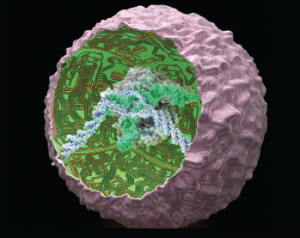
Smart cells were created by genetically reprogramming induced pluripotent stem cells using the CRISPR/Cas9 system to produce biologic drugs in an autoregulated manner.
Ella Marushchenko
The words genetically modified are making people run for the hills these days. Not so when it comes to arthritis care, however.
In the lab of one pioneering researcher, genetic engineering is catapulting arthritis treatment years ahead. Farshid Guilak, PhD, is a professor in the Department of Orthopaedic Surgery at Washington University, St. Louis, and director of research for the Shriners Hospitals for Children in St. Louis. He and his colleagues set out to find a solution to the problem that typically arises with arthritis drugs that attack the inflammation-promoting molecule tumor necrosis factor-alpha (TNFa): too broad an impact.
Dr. Guilak says, “Although current arthritis medications have shown some effectiveness in relieving pain and inflammation, these drugs are delivered system wide instead of being targeted to the affected joints. This creates more problems for patients because their immune systems are left vulnerable to infection. Our goal was to actually edit the genes such that the cells themselves would produce an anti-inflammatory drug.”
Working with colleagues at Duke University and Cytex Therapeutics Inc., they did just that.
Regenerative Approach to Arthritis

Farshid Guilak, PhD
Dr. Guilak, co-director of the Washington University Center of Regenerative Medicine, is co-senior author on the recently published work, “Genome Engineering of Stem Cells for Autonomously Regulated, Closed-Loop Delivery of Biologic Drugs.”1 He explains, “We first took skin cells from the tails of mice and transformed them into pluripotent stem cells, with the eventual goal of creating SMART (Stem Cells Modified for Autonomous Regenerative Therapy) cells.”
Jonathan M. Brunger, PhD, formerly with Duke University, is the paper’s first author. Now a postdoctoral fellow in cellular and molecular pharmacology at the University of California, San Francisco, Dr. Brunger says, “We took advantage of molecular tools that allowed us to rewire how cells respond to input from their environment. In this case, we used the genome engineering tool CRISPR (clustered regularly interspaced short palindromic repeats)/Cas9 to recode how a cell behaves in the context of inflammation.”
Repurposing Inflammatory Pathways
Dr. Guilak, who also has faculty appointments in the Departments of Developmental Biology and Biomedical Engineering at Washington University, elaborates on their process. “When TNF binds to receptors on the cell surface, it stimulates the production of an inflammatory response. We used CRISPR/Cas9 to directly target and inactivate an inflammatory gene, and then insert a gene that releases an anti-inflammatory biologic drug. When the rewired SMART cell encounters TNF, it triggers the production of the drug that blocks TNF. Because the cells are stem cells, we can then convert them to any other cell type, such as cartilage-producing cells—chondrocytes—that can repair damaged joints. This all means that arthritic cartilage is replaced and that joints and other tissues are protected.”