Rheumatoid arthritis (RA) is a systemic autoimmune disease associated with erosive destruction of diarthrodial joints. Patients who are seropositive are more prone to developing extra-articular manifestations, such as rheumatoid lung, rheumatoid nodules and others. With the development of disease-modifying anti-rheumatic drugs (DMARDs), the incidence and severity of these extra-articular manifestations has declined.
Below, we describe a patient with seropositive RA who developed progressive multifocal leukoencephalopathy after aggressive treatment of rapidly progressive constrictive bronchiectasis with rituximab.
Case
Our patient was a 50-year-old man who was a longstanding patient in our rheumatology practice. Historically, he had been diagnosed with seropositive (+ACPA and +RF) juvenile idiopathic arthritis (JIA) at the age of 12. Treatment early in his disease process included steroids, methotrexate and etanercept. Based on documented disease activity scores, he was in a low disease activity state or remission for the majority of his young life. In fact, he was playing 18 holes of golf and repairing woodwind instruments late into his disease process. Additionally, he had a history of monoclonal gammopathy of unknown significance (MGUS) with IgA lambda light chain seen on serum protein electrophoresis with a normal bone marrow biopsy.
He was well controlled on etanercept until 2012. At that time, he developed a rapidly progressive decompensation in his disease process, complicated by shortness of breath. He had never used tobacco, been exposed to secondhand smoke or been exposed to occupational hazards.
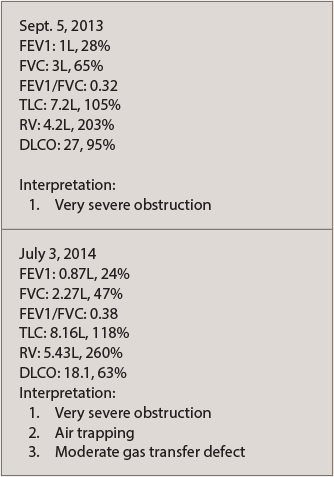
A chest CT scan with contrast noted a left upper lobe subcentimeter nodule that was benign in appearance. A follow-up chest CT in 2015 revealed development of bilateral bronchiectasis, but showed no evidence of interstitial lung disease. He was referred to pulmonology and diagnosed with obstructive lung disease due to rheumatoid arthritis (see PFTs in Table 1).
He was started on conventional medications for chronic obstructive pulmonary disease, which provided only minimal benefit. He was then referred to the Mayo Clinic in Jacksonville, Fla. for a second opinion. He was given the diagnosis of rapidly progressive constrictive bronchiectasis, associated with his RA, in which the smallest airways can become obstructed due to inflammation. This disease is potentially fatal if left untreated. The doctors at the Mayo Clinic recommended against a lung biopsy due to his tenuous pulmonary status.
The etanercept was discontinued, and he was started on an RA-guided regimen of rituximab. He was given a total of two-and-a-half cycles of rituximab before he developed numerous neurological deficits, including left-sided hemiparesis, confusion and ataxia. He was admitted to the hospital for further evaluation.