NEW YORK (Reuters Health)—Sialendoscopy with irrigation of the major salivary glands can enhance salivary flow and reduce xerostomia in patients with Sjogren’s syndrome, according to a randomized trial.
“In our study it is suggested that patients with recent onset of Sjogren’s syndrome and with residual salivary gland capacity could benefit from sialendoscopy,” said Dr. Derk Hendrik Jan Jager from VU University Medical Center, in Amsterdam.
“Therefore, early recognition and diagnosis of Sjogren’s syndrome are essential, and sialendoscopy should be offered as soon as possible as an adjuvant or alternative treatment in reducing oral dryness and to prevent or postpone the consequences of hyposalivation,” he told Reuters Health by email.
Sjogren’s syndrome (SS), an autoimmune disorder affecting the exocrine glands, causes a gradual reduction in the quantity and quality of saliva. There is no effective treatment for SS or the hyposalivation that it causes.
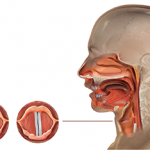
Dr. Jager’s team investigated the effect of sialendoscopy with saline irrigation or saline/corticosteroid irrigation on salivary function, oral dryness and symptoms in their randomized trial of 49 patients with SS.
Among the 16 patients who underwent sialendoscopy followed by saline irrigation, all but two (87.5%) experienced improvements in unstimulated saliva flow and 12 (75%) experienced improvements in stimulated saliva flow at 24 weeks, the researchers report in Annals of the Rheumatic Diseases, online February 23.
Improvement rates were somewhat lower among the 18 patients who underwent sialendoscopy followed by saline/corticosteroid irrigation (72.2% for unstimulated saliva flow and 61.1% for stimulated saliva flow).
Outcome measures did not change significantly among the 15 patients assigned to the control group.
About two-thirds of patients in both sialendoscopy groups regained adequate unstimulated salivary flow after 24 weeks, whereas 37.5% in the saline group and 55.6% in the saline/corticosteroid group regained adequate stimulated salivary flow.
Xerostomia Inventory scores improved in both sialendoscopy groups, suggesting that the intervention resulted in a reduced dry mouth feeling, but only the differences between the saline group and controls were significant.
Both sialendoscopy groups showed greater improvements than controls in EULAR Sjogren’s Syndrome Patient-Reported Index (ESSPRI) scores.
“In our study sialendoscopy was performed under general anesthesia, which could be an impediment for both patients and physicians,” Dr. Jager said. “We would like to emphasize that sialendoscopy is a minimally invasive procedure that can easily be performed under local anesthesia. This is currently done in our department. The complication rate is low, and the treatment is well tolerated.”