Antiphospholipid syndrome (APS) is an autoimmune clotting disorder that may present catastrophically with multiple thromboses over a short period of time. In this article, we examine the case of a woman with undiagnosed APS whose first symptoms presented during a long-haul flight. A review of the literature on thrombosis at high altitudes and during long duration travel helps us understand potential treatment and prevention of the same in APS patients.
Clinical Vignette
A 22-year-old woman noted diffuse severe abdominal pain while traveling by plane from California to India. Each episode began with a bloating sensation that progressed to cramping pain with nausea but no emesis, no relation to food intake and eventual resolution of symptoms without intervention. Such symptoms recurred with any long flights she took, typically to and from India.
One year later, a comprehensive evaluation, including negative infectious workup, yielded the diagnosis of irritable bowel syndrome and cholelithiasis without cholecystitis. After undergoing an elective cholecystectomy, her postoperative course was complicated by renal infarction (see Figure 1A) followed by splenic (see Figure 1B), ovarian and mesenteric infarction within one week. Serologic examination was significant for elevated serum cardiolipin antibody titers, yielding a diagnosis of catastrophic antiphospholipid syndrome.
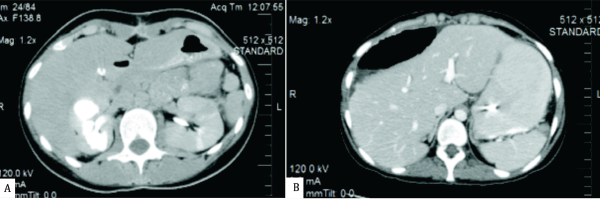
Figure 1
She was subsequently treated with anticoagulation in addition to plasmapheresis and rituximab. However, the question of prior symptoms then arose: Was her initial abdominal pain actually mesenteric ischemia? Could this have been prevented?
The Clinical Problem
Although vast numbers of individuals travel by air yearly, many remain unaware of the risk of deep vein thrombosis (DVT) and venous thromboembolism (VTE) posed by time spent at high altitudes with prolonged immobility, even in healthy individuals. Those with hypercoagulable conditions, such as APS, are at even greater risk. The literature describing the clotting risk with prolonged travel (typically greater than eight hours) is extensive.1 However, limited data describe a specific association between clotting risk and high altitudes in patients with APS. For this reason, we conducted a literature review to evaluate the association of high altitudes and clotting in patients with APS, in addition to management recommendations in such situations.
The Evidence
Individuals ascending to altitudes greater than 2,400–3,000 meters have demonstrated hypobaric hypoxia and its effects on the coagulation system, including decreased tissue oxygenation and sympathetic compensatory changes.2,3 In 2006, Peter Bärtsch, MD, described healthy mountaineers suffering from altitude-induced thrombosis and subsequent death.4 Hypoxemia activates transcription factor early growth response-I (EGR-1), which results in vascular fibrin deposition. This is amplified by a concomitant suppression of fibrinolysis by upreguation of plasminogen activator inhibitor-1.5
