Want to know more about vasculitis in the nervous system? Check out these abstracts from Arthritis & Rheumatism, and log on to www.wileyonlinelibrary.com/journal/arthritis to read the full articles.
Giant cell arteritis: Involvement of intracranial arteries. (Arthritis Rheum. 2006; 55:985-989.)
Introduction
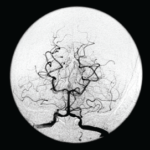
Cerebrovascular ischemic events have been reported in 3% to 4% of patients with giant cell arteritis (GCA). Clinical and pathologic findings suggest that these ischemic events are due to involvement of extradural vertebral and carotid arteries with high-grade stenosis or occlusion rather than intracranial vasculitis.
Several previous reports have described patients with cerebral vasculitis who were also considered to have GCA. However, most of these patients probably represent cases of primary central nervous system vasculitis (PCNSV), a different disease with similar histopathologic findings. To determine the occurrence and frequency of central nervous system (CNS) vasculitis in GCA, we reviewed the medical records of all patients with a diagnosis of CNS vasculitis or angiitis at the Mayo Clinic (Rochester, MN) over a 17-year period and identified those with both biopsy-proven GCA and pathologic and/or angiographic evidence of intracranial vasculitis.
Primary central nervous system vasculitis with prominent leptomeningeal enhancement: A subset with a benign outcome. (Arthritis Rheum. 2008; 58:595-603.)
Abstract
Objective: Primary central nervous system vasculitis (PCNSV) is an uncommon condition that affects the brain and spinal cord. This study was undertaken to evaluate the clinical features and outcomes among patients with PCNSV who presented with prominent gadolinium meningeal enhancement on magnetic resonance imaging (MRI).
Methods: Through retrospective review using the Mayo Clinic medical records linkage system, we identified 101 consecutive patients with PCNSV based on brain biopsy or conventional angiography (or both) between January 1, 1983 and December 31, 2003. We evaluated data on demographics, clinical findings, laboratory studies, imaging, biopsy of brain or spinal cord (or both), treatment, and neurologic outcome.
Results: MRIs showed prominent leptomeningeal enhancement in eight of 101 patients with PCNSV. In six of those eight, cerebral angiography or magnetic resonance angiography results were normal, but biopsy of the brain or spinal cord showed vasculitis in all eight. Granulomatous vascular inflammation was found in six specimens and was associated in four cases with vascular deposits of beta-amyloid peptide. All eight patients had a prompt response to therapy, with resolution of the MRI meningeal enhancement. Although three of the eight patients had relapses during followup, the overall outcome was favorable. Patients with meningeal enhancement, compared with patients without enhancement, more commonly had substantial abnormalities of cerebrospinal fluid (100% versus 58%; P=0.02) and amyloid angiopathy (50% versus 12%; P=0.03).