Editor’s note: Read more about this research in a paper by Dr. Pincus and colleagues in our sister publication, Arthritis Care & Research.
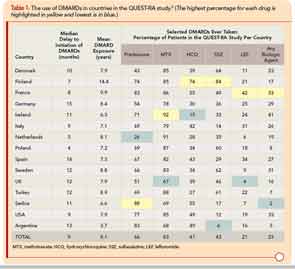
Textbooks of rheumatology and recommendations of professional societies have long suggested that glucocorticoids in rheumatoid arthritis (RA) should be used primarily as “bridging therapy,” while awaiting the benefits of disease-modifying antirheumatic drugs (DMARDs), and/or in acute emergencies such as life-threatening vasculitis or vision-threatening scleritis. Recent EULAR recommendations reflect this directive.1 Nonetheless, many RA patients treated by rheumatologists take low-dose prednisone on a long-term basis. For example, in the international database of the Quantitative Clinical Assessment of Patients with Rheumatoid Arthritis (QUEST-RA) study, among 4,363 RA patients seen in usual care at 48 clinical sites (approximately 100 patients per site) in 15 countries, 66% of consecutive patients took glucocorticoids, including more than 70% in Argentina, Finland, France, Ireland, Serbia, and U.S., and more than 50% in seven other countries—all but Denmark (43%) and the Netherlands (26%) (see Table 1).2 Therefore, rheumatologists’ experience suggests that long-term prednisone may be desirable for many, if not most, patients with RA.
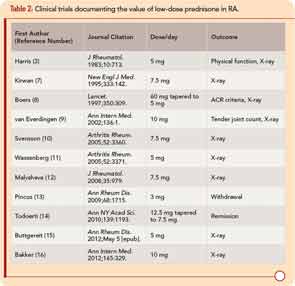
Extensive use of low-dose prednisone at this time appears based in part on a reassessment of glucocorticoid therapy that began during the 1980s, with concurrent recognition of severe long-term outcomes of RA.3-5 The efficacy and safety of low-dose prednisone was documented in an open study reported in 1964, and a 24-week clinical trial reported in 1982.3,6 Since 1995, 11 double-blind RA clinical trials have provided strong evidence for the efficacy and safety of prednisone in doses of 10 mg/day or less over two years or less compared to a placebo.7-16 A withdrawal clinical trial documented clinical efficacy of prednisone in doses of 3 mg/day compared to placebo (see Table 2).13 Disease-modifying properties of low-dose prednisone or prednisolone of 5 mg/day, confirmed in meta-analyses, are of particular interest, as doses of 7.5–10 mg/day are associated with adverse effects and outcomes, including bone loss and higher mortality rates.3,11,17-22
I have summarized treatment of RA patients with prednisone over 25 years between 1980 and 2004 at a weekly academic clinical setting, almost always with concomitant methotrexate after 1985.23-25 A database of all visits of all patients included medications; scores on a multidimensional health assessment questionnaire (MDHAQ) for functional status, pain, and routine assessment of patient index data (RAPID3); and self-report of possible adverse effects.26
