Denial of claims is one of the most unpredictable processes in the billing system for physician practices. Most practices lose thousands of dollars each year due to lack of follow-up or writing off denied claims incorrectly. According to The Physician Billing Process: 12 Potholes to Avoid in the Road to Getting Paid, it costs a physician practice approximately $15 per claim to rework a denied service, which includes staff time, interest, and overhead.1 It is crucial for physicians and their staffs to stay on top of denials to keep the revenue cycle flowing properly and avoid unnecessary administrative burdens.
Physician practices must look more closely at what denial management is and what is needed. Reports have shown that more and more physician practices are turning to denials management to maximize their bottom dollar. The reason is that there is a 5% to 8% denial rate in most practices nationwide and reports show that 50% of denied claims are never refiled. In denials management, 90% of denials are preventable, and 67% are recoverable. This means, in a practice with a $1,000,000 revenue stream, denials potentially represent between $50,000 and $80,000 in lost revenue. Given the magnitude of the numbers, a targeted strategic plan for denials management is necessary to minimize losing large sums of money, resulting in a significant revenue increase to the typical practice.
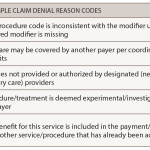
The first step in the process is to create a denials management team, even if it is a team of one. However, ideally it should include billers, coders, and practice managers. The denials management team will need to be proficient in analyzing data and creating reports, and knowledgeable about the coding and billing process. A complete understanding of payer policies and denial codes is very important, as each member of the team will need to know how to decipher the denial explanation codes that are used by Medicare and third-party payers.
Regardless of the approach, denials management is typically time and resource intensive to implement. If you make the commitment to implement denials management using only resources internal to the practice, you must be prepared to:
- Make decisions in advance on which payers will be targeted monthly or quarterly. It will be necessary to create reports to define the denial reasons, as well as what information systems changes need to be made.
- Denials will need to be categorized and separated to identify the most frequent denial codes by payers and procedures. If you are in a multispecialty or physician group, denials can be separated by physician.
- Create a process to resubmit claims with necessary documentation.
- Prepare an implementation plan that details each of the activities needed to complete and refile claims.
- Develop a plan to gather the fee schedule information that you need.
- Identify reports that will be used to monitor efforts and outcomes.
- Communicate the importance of the project to all relevant clinical and nonclinical staff.
- Define process, benchmark performance targets, timetables, and performance standards for those employees charged with the daily charge entry, billing, follow-up, and reporting duties for claims resubmitted for payment.
- Anticipate and budget as needed for additional staffing and related expenses associated with the additional claims follow-up, management, and reporting duties.
If claims are continuously denied, staff will need to learn individual payers’ appeals processes. For Medicare, the appeals process is available at www.cms.hhs.gov/OrgMedFFSappeals. Remember that each private payer has its own process for appealing denied claims and it is important for your staff to access the payer’s appeals process from their website or through your account representative. See the figure above for a simple, five-step process to appeal a denied claim.