SAN DIEGO—Rheumatologists may encounter patients with systemic disease who present with various forms of alopecia that seem sudden or unusual. Hair loss can be caused by autoimmune inflammation in some cases, but there are many other potential causes that a rheumatologist must explore to treat the condition effectively.
Rheumatologists often may see a patient presenting with a complaint of hair loss, especially those with autoimmune diseases like systemic lupus erythematosus (SLE) or rheumatoid arthritis (RA), said Maria K. Hordinsky, MD, chair of the department of dermatology at the University of Minnesota in Minneapolis during her presentation at the 2013 ACR/ARHP Annual Meeting. “Even though you have done a great job of treating their connective tissue disease,” alopecia can still occur. [Editor’s Note: This session was recorded and is available via ACR SessionSelect at www.rheumatology.org.]
Hair Sheds Daily
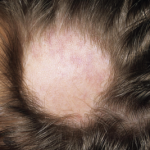
Looking at a cross-section image of a normal scalp, about 90% of the hair follicles look the same, Dr. Hordinsky said. However, hair shedding and even pattern baldness are common among almost all adults. “Every day, we shed hair fibers. There is always recycling going on,” she said. Hair production goes through three cycles: anagen (actively growing), catagen (involution of growth), and telogen (resting). Telogen effluvium is the general term for pattern hair loss. “When patients come to you complaining that their hair is coming out at the roots, what they are losing are the telogen fibers,” she said. Stem cells are located in the bulge region near the base of the hair follicle, she noted.
Alopecia has a psychological impact for many patients, and they may try to hide their hair loss with caps, scarves, or hairpieces. It’s important for rheumatologists to not assume telogen effluvium is simply female pattern baldness but to examine the scalp closely and consider many possible causes, Dr. Hordinsky said. Ascertain if the patient’s family has a history of baldness, and also check for nail abnormalities, menstrual irregularities, or pregnancy, as well as asking about excess body hair, which the patient may have waxed or shaved, she suggested.
Looking closely at the scalp for symptoms like burning, pruritus, pain, redness, scaling, folliculitis, or scarring may provide more clues to the cause of the hair loss. Look at the pattern of hair loss as well as whether or not there is new hair growth visible. A “pull test” is standard. If six or more hairs from any site on the scalp fall out with gentle pulling, this is a sign of diffuse alopecia areata (AA), an autoimmune disease, she said. Standardized scales help categorize the level of alopecia; female pattern baldness is measured on the Ludwig scale, and male pattern baldness is measured on the Hamilton-Norwood scale.