THE CASE:
A 65-year-old man with a history of psoriasis presents to the emergency department with a three-day history of subjective fever, polydipsia, and swelling of his face and extremities. Current medications: adalimumab and moxifloxacin.
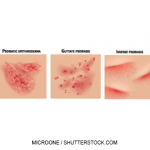
His vital signs are remarkable for temperature of 100.3°F and tachycardia at 122 beats per minute. His skin is noted to have a generalized beet-red, scaling rash that covers the majority of his body (see Figures 1 and 2, right). Severe anasarca is noted and was most pronounced in his face and extremities (see Figures 3 and 4, below right).
The patient’s labs demonstrate a white blood cell count of 10.7×109 L and an elevated lactic acid of 5.8 mmol/L. The electrolyte panel shows evidence of acute renal insufficiency, with a creatinine of 2.45 mg/dL, and the albumin is noted to be low at 2.7 g/L. Chest X-ray and urinalysis are normal.
Diagnosis
The patient’s presentation is consistent with an erythrodermic psoriasis flare.
Erythrodermic psoriasis is the most severe form of psoriasis and is potentially life threatening. It is characterized by a widespread, fiery erythematous rash and exfoliation often affecting the majority of the patient’s skin. Severe itching and pain, fluctuating body temperatures and tachycardia are common.1



Acute management focuses on restoring intravascular volume, managing anasarca and monitoring temperature instability. Recent research indicates that such medications as intravenous cyclosporine and infliximab that regulate epithelial cell growth and immune system response are usually effective, but therapy will be dictated by the patient’s condition and comorbidities.2 Secondary infection and development of septic shock can cause significant morbidity and mortality with erythrodermic psoriasis flares. Therefore, evaluation for underlying infection is critical.3
To restore the patient’s intravascular volume, he is given aggressive intravenous hydration with normal saline. A 500 mL 5% albumin solution is also infused to mitigate the anasarca and hypoalbuminemia. Vital signs are monitored, and his tachycardia gradually resolves. The patient is pan cultured, and after consultation with the patient’s dermatologist, the patient is admitted to the hospital and started on intravenous cyclosporine.
During his hospital stay, the patient is seen by the infectious disease and nephrology services. The patient initially responds favorably to therapy, but subsequently develops worsening renal insufficiency, and the cyclosporine is discontinued in favor of adalimumab. The patient is started on intravenous antibiotics because some of the involved areas of skin appeared cellulitic.