ACR Convergence 2020—In May 2020, the ACR published its updated guideline for the management of gout.1 It followed on the heels of a 2017 gout guideline published by the American College of Physicians.2 Although the guidelines provide similar recommendations on the treatment of acute gout, they differ importantly in the use of uric acid-lowering therapy for long-term management of gout. In a session titled Evidence-Based Guidance for Optimizing Gout Management, Robert Terkeltaub, MD, chief of rheumatology at the VA Medical Center San Diego, professor of medicine in the Division of Rheumatology, Allergy and Immunology at the University of California, San Diego, and president of the Gout, Hyperuricemia and Crystal-Associated Disease Network (G-CAN), discussed these differences and highlighted the evidence that continues to support the ACR recommendations on uric acid-lowering and treat-to-target strategies for managing chronic or tophaceous gout.
In a session titled Evidence-Based Guidance for Optimizing Gout Management, Robert Terkeltaub, MD, chief of rheumatology at the VA Medical Center San Diego, professor of medicine in the Division of Rheumatology, Allergy and Immunology at the University of California, San Diego, and president of the Gout, Hyperuricemia and Crystal-Associated Disease Network (G-CAN), discussed these differences and highlighted the evidence that continues to support the ACR recommendations on uric acid-lowering and treat-to-target strategies for managing chronic or tophaceous gout.
Calling the new evidence weighed by the 2020 ACR updated guidelines “robust,” Dr. Terkeltaub provided an assessment of the new data supporting the strong benefits of lowering uric acid levels on reducing joint structural effects and damage (e.g., synovitis and erosions), reducing the uric acid burden (e.g., uric crystal deposits in tissue) and managing symptoms (e.g., acute flares). “These are all significant and impactful benefits that justify a uric acid-lowering approach in more patients, as well as a treat-to-target strategy,” he said. Table 1 (below) highlights the results of the key evidence he discussed.
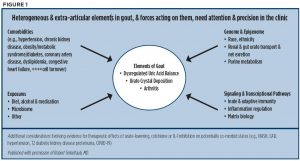
Some unknowns remain: One important question not addressed in the guideline is how to more quickly prevent or limit synovitis and joint damage, including erosions. Another is what the impact of achieving targeted uric acid levels is on the whole patient. Dr. Terkeltaub discussed remaining gaps in the clinical care of gout and emphasized the important role of pharmacogenetics to arrive at a more precise way to treat patients (see Table 2, bottom). He also provided a graphic showing the heterogenous elements of gout that need attention to provide more precise and personalized management of gout (see Figure 1).
Treat the Whole Person
Dr. Terkeltaub believes answers to these questions will be forthcoming, particularly given the work being done in providing good molecular pharmacogenomics. Citing the use of the HLA-B*5801 gene test to predict severe allopurinol hypersensitivity syndrome to identify patients to whom allopurinol should not be given, he underscored the growing interest in, and understanding of, the ABC transporter gene ABCG2 and whether it and its variant, Q141K ABCG2, may offer similar benefits for gout management.