Psoriatic arthritis (PsA) has a higher life impact on women than men, suggesting the need to include life impact as part of the treat-to-target strategy for PsA. This is the finding of a recently published study by Orbai et al., which found female sex independently linked to high PsA life impact.1
The Study
The study was undertaken to better understand sex differences in treat-to-target status, disease activity and patient-reported outcomes in patients with PsA, and assess the association of sex on life impact. Prior studies showing different PsA phenotypes and outcomes between men and women with PsA suggest the need for a more tailored approach to treatment based on sex.
Using data from the Remission and Flare in PsA Study (ReFlaP), an international study of patients with established PsA, Orbai et al. assessed the association between life impact and sex in patients with PsA. The ReFlaP study included 466 consecutive adult patients enrolled in 21 centers and 14 countries who underwent a comprehensive PsA assessment that included scoring of Disease Activity in Psoriatic Arthritis (DAPSA), minimal disease activity and Psoriatic Arthritis Impact of Disease (PsAID).

Dr. Orbai
Included in the current trial were data on 458 patients (for whom complete data on sex was available), of whom 230 (50.2%) were men. Patients had a mean age of 53 years and a mean disease duration of 11 years, and 51.5% were taking a biologic disease-modifying anti-rheumatic drug (bDMARD).
The investigators used a new measurement provisionally endorsed by Outcome Measures in Rheumatology (OMERACT)—the PsAID12 tool—to measure specific, health-related quality of life of these patients with PsA.
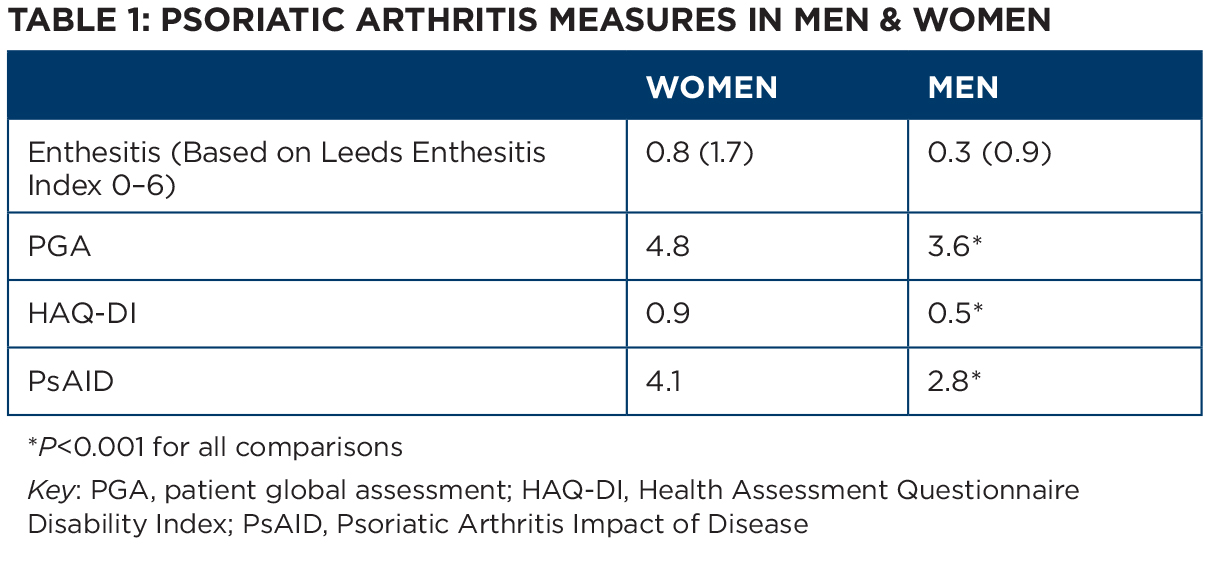
Tables 1 and 2 list key differences in outcomes based on sex. As shown in Table 1, significantly more women had enthesitis and adverse patient-reported outcomes. As shown in Table 2, 37.8% of the 57.1% of patients meeting the criteria for remission or low disease activity achieved minimal disease activity. However, women reached minimal disease activity significantly less than men (25.7% vs. 50%). In addition, women had higher DAPSA scores than men (16.9% vs. 12.6%).
Using these data, the investigators then constructed a number of regression models to assess the link between sex and life impact of PsA. Using a simple regression model adjusted for age and disease duration, they found a significant association between female sex and high PsAID score independent of follow-up time between consecutive visits (odds ratio 2.71; 95% CI 1.85–3.97; P<0.001).
Building on this model, they developed a multivariate regression model adjusted for sex, number of comorbidities, age, disease duration, musculoskeletal disease activity (i.e., SJC66, 68 tender joint count [TJC68], Leeds Enthesitis Index [LEI]), skin disease activity (BSA>5%), systemic inflammation (CRP mg/dL continuous value), and use or nonuse of a biologic, and found a number of variables significantly linked to high life impact (see Table 3).
The investigators constructed separate regression models for each sex in which an independent association between life impact with TJC68 was found in both men and women, but was stronger for women (see Table 4). These analyses found different factors independently associated with high impact for women and men. For women but not for men, follow-up time and biologic use independently decreased life impact, whereas severe psoriasis increased life impact. For men and for women, TJC68, LEI and comorbidities were independently linked to life impact.