On May 1, after their annual scientific meeting in Chicago, the American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons updated its guidelines for this patient population.1,2 One of the primary changes is a move away from using nonsteroidal antiinflammatory drugs (NSAIDs), either cyclooxygenase-2 inhibitors or traditional NSAIDs. The original guidelines, published in 2002, recommended that older patients use any NSAIDs (e.g., prescription or over the counter [OTC]) rather than opioids for persistent pain.3 This updated guideline notes a greater risk (e.g., cardiovascular, renal, gastrointestinal [GI]) for using NSAIDs in this patient population. Using newer clinical trial data and data from clinical observations, the panel now recommends that NSAIDs be rarely considered in highly selected older individuals. When they are considered for use, it should be with extreme caution. For these individuals, the guideline recommends using GI protection with a proton pump inhibitor (PPI) or misoprostol, not taking more than one NSAID for pain relief at a time, and routinely assessing for GI and renal toxicity, hypertension, heart failure, and other drug–drug and drug–disease interactions.
Additionally, patients taking aspirin for cardioprophylaxis should not use ibuprofen.
The guidelines recommend using opioids for older patients with moderate to severe pain or pain-induced diminished quality of life, noting that opioids may be potentially safer for long-term use than NSAIDs. The guidelines also recommend using adjuvant therapies for managing refractory pain. For example, the panel recommends avoiding tertiary tricyclic antidepressants (e.g., imipramine, doxepin, amitriptyline) because of a higher risk for anticholinergic and cognitive adverse effects.4 Avoiding the use of tertiary tricyclic antidepressants is relatively consistent with the updated Beers criteria for potentially inappropriate medication use in older patients.5 Additionally, it is imperative to assess bowel function initially and at follow-up in all opioid-treated patients, as constipation and other GI symptoms may occur.3 It is usually appropriate to prescribe a prophylactic bowel regimen for patients who will be on persistent opioid therapy. Physicians should also encourage adequate fluid intake.
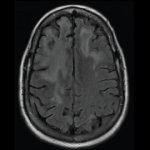
To ensure that patients are aware of the risks and benefits of using mycophenolate mofetil (MMF; CellCept, Myfortic, and generics), Roche and the FDA developed a medication guide that now accompanies every prescription filled for MMF-containing products. One risk includes the possibility of developing of progressive multifocal leukoencephalopathy (PML) (see below).6
New Approvals
- Certolizumab pegol (Cimzia) was approved by the Food and Drug Administration (FDA) for treating moderately to severely active rheumatoid arthritis (RA). Dosed subcutaneously as an initial injection of 400 mg, with 400-mg injections subsequently at two and four weeks, further injections of 200 mg should be administered every other week. Maintenance therapy includes dosing at 400 mg every four weeks. In clinical trials, certolizumab pegol with MTX reduced signs and symptoms of RA at 24 weeks compared with MTX monotherapy.14
- Lansoprazole (Prevacid 24 hours) received FDA approval for OTC use to treat frequent heartburn. It is the second PPI to gain OTC status and should be available later this year.15
Label Changes and Warnings
In May, the Food and Drug Administration (FDA) requested that the manufacturers of all anti-epileptic drugs (AEDs) include a warning in the label of this class of these agents regarding an increased risk of suicidal thoughts and suicidal ideation. Each company will develop a medication guide that explains the risks to patients and that will accompany all filled prescriptions of these drugs (except agents indicated for short-term use). Medication guide updates are expected to be completed by year’s end. It is important for the rheumatology community to be aware of this because patients may have questions about use of these agents and associated risks.