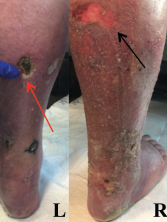
Figure 1: Lower Extremity Ulceration
Varying stages of ulceration are seen on the left (L) and right (R) lower extremities. An eschar formation is on the left (red arrow), and a superficial ulceration is on the right (black arrow).
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis that typically affects medium-sized muscular arteries. The clinical subsets of PAN are idiopathic, generalized, secondary hepatitis B virus (HBV) associated and cutaneous PAN. These clinical subsets are important because of their therapeutic implications.
Virtually any organ system can be affected in generalized PAN, but this vasculitis tends to spare the lungs.1 Pleural effusion, transient infiltrates and bronchial artery vasculitis are uncommon manifestations that have been reported in association with PAN.2 These pulmonary manifestations tend to be a reflection of renal or cardiac insufficiency rather than a direct result of the necrotizing vasculitis.
In the case below, we report on the unusual occurrence of shrinking lung syndrome (SLS) and brachial plexopathy in a confirmed case of PAN. This case highlights a broader consideration for the etiology of dyspnea in PAN and adds to the list of immune-mediated diseases associated with SLS and Parsonage-Turner syndrome (PTS).
Case Presentation
A 51-year-old man presented to the hospital with a four-month history of recurrent, bilateral, lower extremity edema and ulcerations that had been treated with intermittent courses of corticosteroids. The ulcers recurred whenever the corticosteroids were tapered. The patient had experienced fever, dyspnea, orchitis, postprandial abdominal pain, uncontrolled hypertension and intermittent right arm pain during the course of his illness. Just prior to hospitalization he had developed dyspnea. His examination was otherwise unremarkable.
The patient’s past medical history was significant for type 2 diabetes mellitus, hypertension and coronary artery disease. His family history was notable for Sjögren’s syndrome and systemic lupus erythematous (SLE). He had a history of smoking tobacco, but denied alcohol or illicit drug use.
On our initial physical examination, the patient had normal vital signs. Despite his complaints of dyspnea and orthopnea, he had normal pulmonary and cardiac examinations. The muscle strength in his right upper arm was 3/5, and he had pitting edema on his lower extremities.
The examination of the patient’s skin was notable for livedo reticularis and ulceration of the lower extremities, extending from the calves to the heels of his feet (see Figure 1, above). The ulcers were of varying stages, with some being early stage and superficial, and other lesions deep with eschar formation.
Laboratory analysis is listed in Table 1.
Table 1: Laboratory Test Results
| Laboratory | Test Result* | Reference Range |
|---|---|---|
| White cell count | 11.6 K/uL | 4.8–10.8 K/uL |
| Serum eosinophil % | 0.036 | 0.0–6.1% |
| Serum eosinophil (number) | 0.4 K/uL | 0.0–0.4 K/uL |
| Hemoglobin | 12.4 g/dL | 14–18 g/dL |
| Platelet | 385 K/uL | 140–420 K/uL |
| Serum creatinine | 0.9 mg/dL | 0.6–1.3 mg/dL |
| Aspartate aminotransferase (AST) | 21 IU/L | 15–41 IU/L |
| Alanine aminotransferase (ALT) | 35 IU/L | 12–63 IU/L |
| Creatine phosphokinase (CPK) | 110 IU/L | 25–250 IU/L |
| C-reactive protein | 1.63 mg/dL | 0–0.6 mg/dL |
| Erythrocyte sedimentation rate | 62 MM/HR | 0–15 MM/HR |
| Anti-nuclear antibody (ANA) | 1:640 titer (nucleolar) | <1:80 titer |
| Anti-proteinase 3 (anti-PR3) | <3.5 U/mL | 0.0–3.5 U/mL |
| Anti-myeloperoxidase (anti-MPO) | <9.0 U/mL | 0.0–9.0 U/mL |
| Anti-double-stranded DNA (anti-dsDNA) | Negative | Negative |
| Interleukin-6 | 2.4 pg/mL | 0.0–15.5 pg/mL |
| Interleukin-2 | <31.2 pg/mL | 0.0–31.2 pg/mL |
| IgE, Total | 779 IU/mL | 6–495 IU/mL |
| C3 complement | 117.0 mg/dL | 90–180 mg/dL |
| C4 complement | 28.0 mg/dL | 10–40 mg/dL |
| Hepatitis B surface antigen | Nonreactive | Negative |
| Hepatitis C antibody | Nonreactive | Nonreactive |
| HIV screen (AB/AG combo) | Nonreactive | Nonreactive |
| B-type natriuretic peptide | 12 pg/mL | 0–100 pg/mL |
| Urine blood | Negative | Negative |
| Urine protein | Negative | Negative |
| *abnormal findings indicated in bold |


