 Granulomatosis with polyangiitis (GPA) is a primary, necrotizing granulomatous vasculitis, involving small- to medium-sized arteries, that causes systemic disease. Almost any organ can be affected, but the most affected systems are the upper airways, lungs, kidneys, eyes and peripheral nerves. Migratory polyarthritis is reported in approximately 25% of patients with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV); however, it’s rarely reported as the initial presenting symptom.1,2
Granulomatosis with polyangiitis (GPA) is a primary, necrotizing granulomatous vasculitis, involving small- to medium-sized arteries, that causes systemic disease. Almost any organ can be affected, but the most affected systems are the upper airways, lungs, kidneys, eyes and peripheral nerves. Migratory polyarthritis is reported in approximately 25% of patients with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV); however, it’s rarely reported as the initial presenting symptom.1,2
Here, we present a case of GPA with migratory polyarthritis as the initial manifestation.
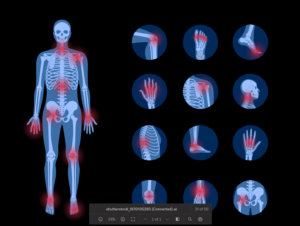
History of present illness: A 49-year-old man without significant medical history presented to the rheumatology clinic for evaluation of polyarthritis that had started eight months before. He reported three episodes of migratory polyarthritis, involving different joints each time (i.e., shoulders; elbows and wrists; knees, and ankles). During each episode, he noted joint swelling, redness (see Figures 1A and 1B), stiffness and pain; his symptoms lasted for five days and then resolved after he received a course of glucocorticoids.
During the second flare, he experienced redness, pain and floaters in both eyes, which also improved with glucocorticoids. He was subsequently seen by an ophthalmologist, who diagnosed him with bilateral iritis.
Additionally, he described chronic low back pain that worsened with exercise and prolonged morning stiffness that he’d experienced for a few years.
Three weeks before his rheumatology visit, he visited the emergency department for evaluation during an inflammatory flare. Plain X-ray films of his ankles showed mild to moderate soft tissue swelling without evidence of acute fracture or osseous abnormalities.
Laboratory tests are summarized in Table 1.
He was discharged on a glucocorticoid regimen and was referred to a rheumatology clinic.
Past medical history & medications: The patient had no pertinent, previous medical history or surgery. The patient’s medications were 10 mg of prednisone daily and 800 mg of ibuprofen twice daily as needed. He denied any recent antibiotic or other medication use, herbal use or vaccination.
Social & family history: He reported no family history of psoriasis, rheumatoid arthritis (RA), inflammatory bowel disease (IBD) or other autoimmune conditions. He has been smoking one pack per day for 10 years. He consumes alcohol socially and denies using any recreational drugs, such as cocaine or heroin. He has lived in Ohio with the same female partner for many years, with no recent travel.



