Background/Purpose
Polymyalgia rheumatica (PMR) is typified by pain and stiffness of the shoulder and hip girdles. Previous qualitative studies have highlighted the importance to patients of additional symptoms, including fatigue and sleep disturbance. These features of PMR are less recognized by clinicians and have not yet been quantified in the literature. Further, the adequacy of the current treatment paradigm in addressing these symptoms is unknown.
Methods
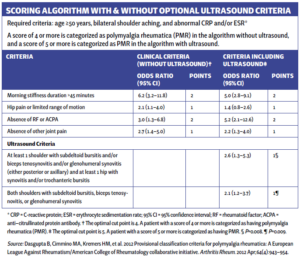
Patients with a new diagnosis of PMR fulfilling 2012 EULAR/ACR Provisional Classification Criteria (see table) were prospectively recruited, together with age- and gender-matched controls. Assessments were undertaken three months after the commencement of corticosteroid therapy, when it was considered likely that inflammatory disease would be controlled.
PMR disease activity was assessed using the PMR-Activity Score (PMR-AS). Patient-reported outcomes were used to assess fatigue (BRAF-MDQ), sleep (PSQI), anxiety and depression (HADS). The two-sample t-test and Mann-Whitney U test were conducted to compare scores in PMR participants against control participants.
Results
From April 2019 to August 2021, 36 participants with PMR and 32 control participants were recruited. The mean age of PMR participants was 68.7 (standard deviation [SD] 8.3) years, and 18 (50%) were women. The mean duration of steroid therapy prior to study assessments was 12.8 (SD 2.1) weeks. Disease activity at the time of assessments was low (median PMR-AS 4.1; IQR 1.7, 10.2).
PMR participants had a higher PSQI score than control participants, indicating lower quality sleep (mean 8.8 [SD 4.5] vs. 5.3 [SD 2.9], difference 3.6 [95% CI 1.8–5.4], P<0.001). The median BRAF score in PMR participants was higher than in control participants (22 [IQR 2, 32.5] vs. 6 [IQR 2, 14.5], P=0.004). Median HAD depression and HAD anxiety scores were also higher in PMR participants (3 [IQR 2, 7] vs. 1 [IQR 0, 3], P<0.001; and 5 [IQR 3, 8] vs. 2 [IQR 0, 3.5], P<0.001 respectively).
Conclusion
Despite treatment-induced low disease activity at the time of assessment, PMR participants had significantly higher levels of fatigue, anxiety, depression and poorer quality of sleep than control participants. These results support previous insights from qualitative studies and underscore shortfalls of the current treatment approach based on corticosteroid monotherapy. Future research should explore risk factors and both pharmacological and nonpharmacological management strategies.
The Study Abstract
From ACR Convergence 2022
Leung J, Owen C, Liew D, Buchanan R. Persistence of fatigue, sleep disturbance and mood disorders in PMR patients despite standard treatment [abstract]. Arthritis Rheumatol. 2022;74(suppl 9).