‘Rheumatologists are increasingly recognizing and treating hyperinflammatory states, but how do we diagnose and treat it? Dr. Nigrovic provides some tips for practical management,’ says Physician Editor Bharat Kumar, MD, MME, FACP, FAAAAI, RhMSUS.
“Macrophage activation syndrome [MAS] can be difficult to identify because it mimics other inflammatory states. However, early recognition and treatment are important to obtain the best outcomes for our patients because MAS can worsen quickly,” says Peter Nigrovic, MD, a rheumatologist at Boston Children’s Hospital, where he is chief of the Division of Immunology, and at Brigham and Women’s Hospital and leads the Center for Adults with Pediatric Rheumatic Illness. He also leads a basic and translational science lab that focuses on the mechanisms of inflammation in arthritis and systemic lupus erythematosus (SLE).
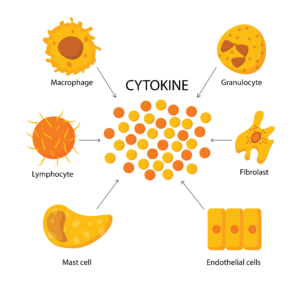
Dr. Nigrovic is the author of a review that is part of a series on immunology for rheumatologists launched earlier this year in Arthritis & Rheumatology.1 In this new installment, Dr. Nigrovic reviews MAS—a cytokine storm potentially leading to life-threatening multisystem end-organ dysfunction—in children and adults, focusing on MAS complications in Still’s disease.2
Practical Approach to MAS
“The goal of this review was to provide a practical approach to [the] diagnosis and treatment [of MAS], starting with basic lab tests easily available to everyone and then incorporating less familiar measurements, such as CXCL9 and interleukin (IL) 18,” Dr. Nigrovic explains. “I have sought to be very specific, including a treatment algorithm and drug dosing recommendations, recognizing that data remain very limited and so other approaches may also be reasonable.”
MAS, a state of immune hyperactivation, occurs in rheumatic diseases, most typically in Still’s disease, which includes systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease; SLE; Kawasaki disease; malignancy, especially leukemia and lymphoma; severe bacterial and viral illnesses; and inborn immunity errors.
“In patients exhibiting a high degree of systemic inflammation, MAS should be suspected early, especially in the context of Still’s disease or other conditions that pose a risk for MAS,” Dr. Nigrovic says. “Measuring ferritin is a good first step, but MAS is characterized by a broader pattern involving other clinical and laboratory features, so looking for other elements of this pattern is important. Sometimes, it makes sense to start treatment for MAS even before you are sure, [because] the ‘MAS vicious cycle’ of reciprocal immune cell activation can spiral out of control.”