The association of RA and the lungs was discussed by Dr. Catrina during her talk, “Lung Inflammation and the Development of RA-Related Autoimmunity.” She presented data from studies showing an association between the presence of specific anti-citrullinated protein antibodies (ACPA) and parenchymal lung abnormalities detected by high-resolution computer tomography, and the presence of local citrullination and anti-citrulline immunity in the lungs early in the development of ACPA-positive RA (see “Key References on Evidence for Lung Inflammation and RA,”).
According to Dr. Catrina, these results suggest that early inflammatory lung events may play a critical role in initiating the development of ACPA-positive RA. “Further studies to address the complex relationship between inflammation in the lungs and in the joints are warranted,” she said. “Such studies will allow identification of environmental factors and early immune events that can be targeted with preventive or therapeutic measures.”
Dr. Scher also emphasized the importance of future studies to validate the current evidence emerging on an association between these mucosal environments and the development of RA by proving causation. “If validated, these findings could lead to the discovery of potential biomarkers and therapeutic approaches at the preclinical and clinical phases of RA,” he said.
Detecting Early Organ Injury in Preclinical Rheumatic Diseases
In a session titled, “Symptom Assessment and Joint Examination in Pre-Clinical Rheumatoid Arthritis: How To Assess in an Accurate, Valid, and Reproducible Fashion?” Vivian P. Bykerk MD, director of the Inflammatory Arthritis Center of Excellence at the Hospital for Special Surgery in New York City, provided information on how to accurately assess symptoms and signs in people at risk for developing inflammatory/rheumatoid arthritis (IA/RA) and how to determine a person’s risk for developing RA based on the presence of certain signs and symptoms.
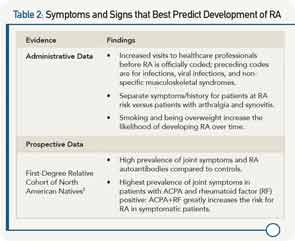
Using information and criteria from recently published recommendations for terminology and research in individuals at risk of RA by the European League Against Rheumatism that define specific phases of RA, she focused her talk on the phase of disease in which patients have symptoms without clinical evidence of arthritis.2 To help clinicians assess these persons at risk for developing RA, she reviewed the current evidence on what symptoms and signs best predict who will develop overt persistent synovitis or classifiable RA (see Table 2).
She also highlighted recent data from imaging studies that show the detection of RA in ACPA-positive patients prior RA diagnosis. A study by Krabben and colleagues conducted to assess whether local inflammation occurs in the preclinical phase of RA found that subclinical inflammation was detected by magnetic resonance imaging in ACPA-positive patients with arthralgia prior to synovitis or even symptoms of RA.4 In another study that examined the relationship between the presence of ACPA and osteoclast differentiation in people with RA-related autoimmunity, Kleyer and colleagues found cortical bone changes (e.g., thinning, fenestration, and small bone erosions) in asymptomatic ACPA-positive people.5