Biologic Therapy for RA
Ronald van Vollenhoven, MD, PhD, professor in the unit for clinical therapy research, inflammatory diseases, at the Karolinska Institute in Stockholm, Sweden, rested his argument on the superior efficacy of biologics as demonstrated in a number of clinical trials (see Table 2). He walked through the data from the one- and two-year results of the Swefot trial, emphasizing that the lack of significantly superior clinical results with the addition of infliximab to MTX compared to the addition of conventional DMARDs to MTX seen at two years could be due to the smaller sample size over time.
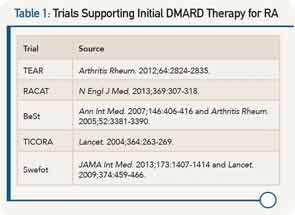
He highlighted data from the OPERA trial that showed that adding a biologic to intensive conventional therapy provided even better outcomes, and that results from the RACAT trial show that conventional therapies can achieve decent responses, but that biologics remain unsurpassed in making some patients do really well and preventing structural damage, as noted by the better radiographic findings with the biologics.
Although he focused more heavily on the efficacy data as the most important evidence on which to base treatment decisions, he did acknowledge the high cost of biologics that prohibit their use in large patient groups. He emphasized the need for a smarter use of biologics, which includes their use in induction-maintenance strategies (i.e., starting patients on a biologic to control disease, but then using conventional therapies for maintenance therapy) and adjusting their dose (i.e., studies indicate that in some patients good results can be achieved with half-dose as opposed to full-dose etanercept).
He also emphasized the need for better personalized approaches to treating patients with RA. “This has been the ‘holy grail’ of therapeutics, to predict at the individual-patient level which drug is the right one for them,” he said. Although he said work is still needed in this area, he mentioned research by his group that suggests the utility of a multibiomarker disease-activity test to identify patients who are and who are not at risk for radiographic joint damage. If the test is confirmed, he said, it could help in choosing the optimal therapy for a given patient.
Overall, Dr. van Vollenhoven said he and Dr. O’Dell agreed more than perhaps the debate format permitted. “Most rheumatologists understand these issues and are dealing with them the best they can,” he said, adding that he hopes he provided some key information that will help clinicians provide the best treatment for each patient.