I have been practicing medicine for 33 years. Wow, 33 years. I am sure many of you are like me in that when you have been practicing this long, some information is ingrained in the depths of your mind. For instance, whenever anyone says rheumatoid arthritis, I know instantly the International Classification of Disease (ICD) code is 714.0. It has been 714.0 for as long as I remember. But moving forward, it could possibly be M05.70, M06.9, or M05.9 because the Centers for Medicare and Medicaid Services (CMS) will be requiring implementation of ICD-10 in 2013. It is time to teach an old dog new tricks beginning with the acceptance of the changes for ICD coding.
What Is ICD-10?
ICD-10 was implemented by the World Health Organization in 1993 and is now used by approximately 25 countries around the world. Why does the United States have to move to ICD-10? One of the major reasons is because the current ICD-9 system is running out of room for new codes. ICD-10 also provides for more detailed codes that will allow for better analysis of diseases and assist in improving treatment outcomes.
How Different Is ICD-10?
There are approximately 14,000 ICD-9 codes, and the codes are mostly numeric with three, four, or five digits. ICD-10 has approximately 68,000 codes, and all the codes are alphanumeric, beginning with a letter and also having a mix of letters and numbers that follow. ICD-10 codes can also go out to a seventh character. ICD-10 will provide more flexibility to add new codes in the future. It now provides codes for laterality and will support the sharing of healthcare data between other countries and the United States.
One of the major reasons the United States is moving to ICD-10 is because the current ICD-9 system is running out of room for new codes. ICD-10 also provides for more detailed codes that will allow for better analysis of diseases and assist in improving treatment outcomes.
How Do You Code ICD-10?
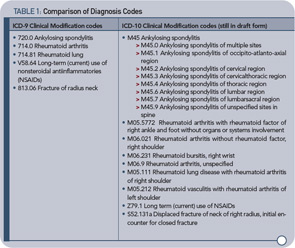
The clinically driven ICD-10 code set has more specific descriptors to better identify diagnoses. Table 1 (below) shows some examples of rheumatology codes that are currently used in ICD-9 and what they will look like in ICD-10.
What Should Our Practice Do to Prepare?
RAND estimates the one-time cost for the United States to convert to ICD-10 at $425 million to $1.15 billion, plus somewhere between $5 million and $40 million a year in lost productivity. Practices need to realize that this is going to happen and start preparing now. The coding system change will affect the basic practice management systems in the office, from the superbills to the electronic medical records to the billing systems. Your office practice manager should take time to review everything that is “touched” by the ICD-9 coding system and realize that everything will need to be changed to be compliant with the implementation date. The ACR is creating a new superbill that physician offices will be able to use to code for ICD-10. However, many practices like to personalize their superbill, so be prepared to make modifications to the sample superbill so it works best for your office’s needs. If you have an electronic billing system, you will need to have new software uploaded to obtain the new codes. Start planning now by creating an implementation plan, including when to contact vendors and communicate with staff. [Editor’s note: See “Plan Now for ICD-10 Changeover” on p. 1 and “ICD-10 from a Coder’s Perspective” on p. 18 for more information on getting your practice ready for ICD-10.]
What Is the ACR Doing to Help My Practice Prepare?
The ACR will have a course at the ACR/ARHP Annual Scientific Meeting in Chicago this November. In 2012, the ACR will offer webinars and additional coding courses. The ACR practice management department is creating a web application tool where physicians can plug in the current ICD-9 code and possible ICD-10 codes will be generated. The Committee on Rheumatologic Care is overseeing the crosswalk to make sure the appropriate rheumatology codes are pulled and placed in one easy location.
Need More Coding Help?
It is important in this reimbursement environment that physicians get the biggest bang for their buck. Physicians need to be coding appropriately (or overseeing coders and billers) to ensure that they receive appropriate reimbursement for the work they have performed. This is becoming even more important as the government expands its audit capabilities. The best way to ensure that you are coding appropriately is to take one of the ACR’s coding courses. The ACR established a coding certification course in conjunction with the AAPC. The Certified Rheumatology Coder (CRHC) exam tests an individual’s ability to read and abstract information from physician office notes, evaluation and management codes, medical terminology, procedures, and rules and regulations regarding Medicare billing. It is interesting that a lot of individuals that think they know coding do not always pass the certification on the first attempt. I highly encourage you to have your coding and billing staff—at a minimum—review the study guide and practice materials for this certification course. It would be unfortunate if you were throwing away money every day due to poor coding.
What’s Next?
Just to keep you on your toes, there are already committees developing the new code sets for ICD-11. The first question that is typically asked is, Why doesn’t the United States just move directly to ICD-11? First, ICD-11 isn’t expected to be released until 2015, which will make it difficult for us to correctly report and categorize diseases in the mean time, because ICD-9 has reached its maximum for codes. With the rise of new health-related conditions as well as new technologies, the United States will need to implement ICD-10 to appropriately report before moving to ICD-11. Think of it this way—one cannot build the second floor of a house before building the foundation. ICD-10 is essentially a required stepping stone to get to ICD-11. Individuals who are familiar with ICD-10 and the changes expected for ICD-11 comment that countries must first implement ICD-10 before moving to ICD-11. The good news is that the ACR is actively involved with the ICD-11 workgroup. ACR member Jonathan Kay, MD, is chairing the rheumatology workgroup to ensure that rheumatology diagnoses are properly classified.
Practicing medicine is becoming a juggling act as CMS tries to throw numerous new regulations at us to see who survives. In just the past few years, physicians have had to adapt to the Physician Quality Reporting System (previously PQRI), electronic prescribing, meaningful use, recovery audit contractors, and more. I guess you can teach an old dog new tricks, after all. The question is quickly becoming, How many tricks can you teach an old dog before he tires out?
For additional information on ICD-10, visit the ACR’s website, www.rheumatology.org/practice, or contact the practice management department at (404) 633-3777 or [email protected].
Dr. Borenstein is clinical professor of medicine in the division of rheumatology at George Washington University Medical Center, in Washington, D.C., and in private practice at Arthritis and Rheumatism Associates there. Contact him via e-mail at [email protected].