Although there is no uniform approach to a diagnosis, the workup for PACNS is never complete without lumbar puncture, Dr. Calabrese advised. Analysis of the cerebrospinal fluid can help rule out infectious mimics. Magnetic resonance angiography with gadolinium enhancement and diffusion-weighted images should be done when a patient has unexplained ischemia; however, the findings can be nonspecific. There is “no angiographic study of 100% specificity for diagnosis of CNS vasculitis,” he said.
A brain biopsy has positive predictive value to rule in the diagnosis, Dr. Calabrese said. With pathology, “you can be far more confident that this is serious business and requires serious medication.” Although a biopsy is not 100% sensitive and can give a false-negative result, it can help rule out other conditions.
The prognosis is usually favorable if a correct diagnosis is made. Although treatment regimens can vary, Dr. Calabrese said that, for the most part, the most serious forms of PACNS can be treated with cyclophosphamides and glucocorticoids. An antimetabolite can be used for maintenance therapy when a disease is in remission.
Mimics of PACNS
Aneesh Singhal, MD, a neurologist at Massachusetts General Hospital and Harvard Medical School, presented diagnostic information about reversible angiitis of the central nervous system (RCVS), a syndrome that can mimic PACNS. Unlike PACNS, which typically affects middle-aged men, RCVS is more commonly seen in women age 20–40. The first symptom often recognized in RCVS is a sudden thunderclap headache or several severe headaches that may or may not be accompanied by neurologic deficits. Triggers can include sexual activity, a recent pregnancy and exposure to vasoactive substances, such as marijuana, cocaine, SSRIs and cough or cold suppressants.
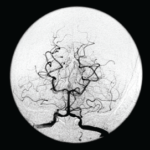
The two conditions have other distinguishing differences, Dr. Singhal said. The cerebrospinal fluid analysis should be normal or nearly normal. The MRI can initially be normal, but about 80% of patients will develop abnormalities over time, and some patients have subarachnoid hemorrhage. “This conversion from normal to abnormal does not occur in PACNS,” Dr. Singhal said. Most importantly for diagnosis is the “sausage-on-a-string” appearance on angiogram, the presence of segmental vasoconstriction in multiple cerebral arteries. RCVS is self-limited, with headaches and vasoconstriction resolving over a period of days to weeks.3 Angiographic abnormalities either completely reverse or substantially reverse within about three months.
Treatment is less aggressive for RCVS than for PACNS, Dr. Singhal said, and usually includes glucocorticoids and calcium channel blockers. Long term, the outcome can include chronic headaches and depression.