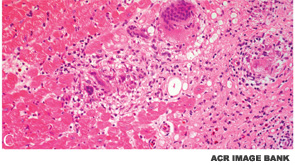
BOSTON—Diagnosis of both cardiac sarcoidosis and neurosarcoidosis requires a process of exclusion and a high degree of clinical suspicion, according to a presentation at the ACR/ARHP Annual Meeting in Boston in November 2014, Sarcoidosis in 2014. Akin to problems associated with the general diagnosis of sarcoidosis, there is no one reliable diagnostic test for either condition, the clinical manifestations can be nonspecific, and there are no evidence-based guidelines for treatment.
Daniel Culver, DO, a pulmonologist at the Cleveland Clinic, said diagnosis of cardiac sarcoidosis can be difficult and should include a finding of sarcoidosis in an organ outside the heart and presence of a heart lesion that cannot be explained by other causes. A patient’s symptoms, however, are still the most important for diagnosis.
“I ask my patients: ‘Are you having palpitations, are you having dizzy spells, have you passed out?’ If any of those things are true, you have to go looking hard for a diagnosis of cardiac sarcoidosis,” he said.
Patients with cardiac sarcoidosis can have congestive heart failure, impaired systolic function, ventricular dysfunction, conduction delays and reduced left ventricular ejection fraction. The symptoms can range from asymptomatic conduction abnormalities to fatal ventricular arrhythmias, depending on the location and extent of granulomatous inflammation.1
Screening for cardiac sarcoidosis should include not only an assessment of the patient’s symptoms, but also an electrocardiogram that can help detect any conduction system abnormalities and whether the heart is involved. Blood test abnormalities are not useful for diagnosis.
Imaging Modalities Used in Diagnosis
No gold standard has been established for imaging cardiac sarcoidosis, and the sensitivity and specificity of imaging modalities are limited. However, contrast-enhanced magnetic resonance imaging (MRI) “does have some utility,” Dr. Culver said. “When you see late enhancement on MRI, that’s a sign that the patient is likely to have some issue. Patients with late enhancement have a worse course.”