BOSTON—The contributions of Stephen Malawista, MD, to the field of innate inflammation and the proinflammatory functions of phagocytes in rheumatic diseases have inspired the work of many researchers, according to Robert Terkeltaub, MD, who gave the Rheumatology Research Foundation Memorial Lectureship, titled Innate Immunity at the Core of Rheumatic Disease, to honor Dr. Malawista at the ACR/ARHP Annual Meeting in Boston in November 2014.
“He posed interesting questions, and the offshoots of his work are felt today. He was a friend and colleague, and he was inspirational,” said Dr. Terkeltaub, professor of medicine at the University of California San Diego and chief of rheumatology at the San Diego Veterans Affairs Medical Center.
Dr. Malawista, now deceased, was chief of rheumatology at Yale School of Medicine for 21 years. He and his team of researchers are credited with uncovering the etiology and pathogenesis of Lyme disease, which pioneered current approaches to better understanding of how microbial organisms play a role in other arthropathies, such as rheumatoid arthritis. Their research, published in the mid- to late 1970s, reported on an epidemic form of arthritis that was clustered in eastern Connecticut and that was believed to be caused by a previously unrecognized clinical entity.1 Subsequent research, published in 1978, reported that erythema chronicum migrans often develops in early Lyme disease and that the disorder was triggered by innate and adaptive immune responses to spirochaetes transmitted by ticks.2
Gouty Arthritis Research
Dr. Terkeltaub said that another of Dr. Malawista’s research passions was acute gouty arthritis. Dr. Malawista elucidated that urate crystals trigger inflammation by inducing IL-1β release from macrophage lineage cells, and he discovered that colchicine quells inflammation by modulating microtubules, he said.

A retrospective report on a half-century of gout research and observations, published by Dr. Malawista and his colleagues in 2011, recounted that their understanding of gout had “moved from inflammatory properties of urate crystals in man to the critical role of neutrophils in the inflammatory process to the governing role of mononuclear phagocytes in the acute attack. … Mononuclear phagocytes appear to be driving the neutrophils throughout the course of the gouty paroxysm,” they wrote.3
Dr. Malawista’s initial work on phagocytes has led to continuing research on innate immunity and inflammation in acute gouty arthritis, Dr. Terkeltaub said. Research by Dalbeth et al demonstrated that the tophus represents a complex and organized chronic inflammatory tissue response to monosodium urate monohydrate crystals involving both innate and adaptive immune cells.4 Coexpression of IL-1β and TGFβ-1 in tophus “suggests that both proinflammatory and antiinflammatory factors present within the tophus contribute to a cycle of chronic inflammation, attempted resolution and tissue remodeling.”
Major Research Developments in Gout
Research related to the role of mast cells in acute gouty arthritis is an important step forward in understanding the disease, Dr. Terkeltaub said, adding that “[Dr. Malawista] would have really loved this work.” Mast cells have been linked with development of acute inflammatory response to monosodium urate (MSU) crystals and development of inflammatory arthritis. “They are markedly activated in acute gouty synovial fluids, especially compared with rheumatoid arthritis,” Dr. Terkeltaub said.

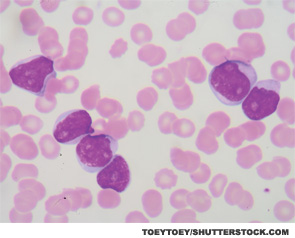
Other research has demonstrated the role of neutrophil extracellular traps (NETs), which are released in innate immunity host responses to both pathogenic organisms and endogenous inflammatory signals. NETs are extruded spider web-like structures in neutrophils with nuclear degradation that are enriched in proteases with the capacity to increase killing microorganisms, damage to vascular and connective tissues, degradation of inflammatory cytokines and generation of citrullinated protein neoantigens. Neutrophils amplify early gouty inflammation through oxidative stress and chemokines, but, at high density, neutrophils also form NETs in response to urate crystals, which is critical in shutting off the acute inflammatory response.
Specifically, research published by Schauer and colleagues showed that MSU crystals induce uncontrolled production of inflammatory mediators from neutrophils and persistent inflammation.5 Using models of neutrophilic inflammation, NETosis-deficient mice developed exacerbated and chronic disease that could be reduced by adoptive transfer of aggregated NETs, they wrote. Their findings suggest that these aggregated NETs “promote the resolution of neutrophilic inflammation by degrading cytokines and chemokines and disrupting neutrophil recruitment and activation.”
The research is important, Dr. Terkeltaub said, because neutrophils have been thought of mainly as “killing machines,” a vital defense system that can phagocytose and kill bacteria and fungi. Now “NETs have been implicated in lupus and vasculitis … and they appear to promote endothelial damage and thrombosis in those diseases.” In contrast, in gout, NETosis is an inflammation “stop signal” and may be a factor in tophus formation and growth, Dr. Terkeltaub said, and “collectively, these developments underscore the work of Malawista and others in how the short-lived neutrophil, even lacking a functional nucleus, has long-lived effects on innate and adaptive immune responses in rheumatic diseases.”
AMP-Activated Protein Kinase (AMPK) & Gout
Understanding how AMPK naturally and therapeutically limits urate crystal-induced inflammation is another important development in gout research, Dr. Terkeltaub said. AMPK is a metabolic biosensor with antiinflammatory activities. “Activated AMPK promotes glucose transport, insulin sensitization, lipid metabolism, the biogenesis of mitochondria and proper function of mitochondria and muscle stamina,” he said. “It is not simply a metabolic super-regulator, but it also suppresses inflammation and oxidative stress. It inhibits inflammatory responses.”6
Tissue AMPK activity is suppressed in gout, however, because of excesses in nutrition and body weight, diabetes and poor physical fitness in many gout subjects, and by likely additional excesses in alcohol consumption and ambient soluble urate in many gout patients. Results of a study published in 2014 by Wang et al demonstrated that AMPK activity not only limits MSU crystal inflammation, but also transduces multiple antiinflammatory effects of colchicine in macrophages.7 “Targeting increased and sustained AMPK activation in inflammatory cells” should be investigated further so the efficacy of prophylaxis and treatment of gouty inflammation could be enhanced, they concluded.
“It is important to recognize that nutrition and fitness have metabolic effects to decrease tissue AMPK activity that are quite pertinent to gout,” Dr. Terkeltaub said. Dietary and alcohol excesses, obesity, diabetes and poor physical fitness all have an effect, whereas nutritional constraint and physical fitness will elevate AMPK activity. Beyond colchicine, several drugs already in the clinic have the potential to limit innate immune inflammation, in large part, by activating AMPK. Those include methotrexate, nonacetylated salicylates, high-dose aspirin and metformin. “There is substantial potential for natural and pharmacologic means to limit harmful innate immune responses more safely and effectively by increasing tissue AMPK activity, such as in gout, osteoarthritis and certain other chronic joint diseases.”
Kathy L. Holliman, MEd, is a medical writer based in Beverly, Mass.
Second Chance
If you missed this session, Innate Immunity at the Core of Rheumatic Disease, it’s not too late. Catch it on SessionSelect: http://acr.peachnewmedia.com/store/provider/provider09.php.
References
- Steere AC, Malawista SE, Snydman DR, et al. Lyme arthritis: An epidemic of oligoarticular arthritis in children and adults in three Connecticut communities. Arthritis Rheum. 1977;20(1):7–17.
- Steere AC, Broderick TF, Malawista SE. Erythema chronic migrans and Lyme arthritis: Epidemiologic evidence for a tick vector. Am J Epidemiol. 1978;108(4):312–321.
- Malawista SE, de Boisfleury AC, Naccache PH. Inflammatory gout: Observations over a half-century. FASEB J.2011;25(12):4073–4078.
- Dalbeth N, Pool B, Gamble GD, et al. Cellular characterization of the gouty tophus. Arthritis Rheum. 2010;62(5):1549–1556.
- Schauer C, Janko C, Munoz LE, et al. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat Med. 2014;20(5):511–517.
- Zhao X, Petursson F, Viollet B, Lotz M, et al. Peroxisome proliferator-activated receptor γ coactivator 1α and FoxO3A mediate chondroprotection by AMP-activated protein kinase. Arthritis Rheumatol. 2014;66(11):3073–3082.
- Wang Y, Viollet B, Terkeltaub R, Liu-Bryan R. AMP-activated protein kinase suppresses urate crystal-induced inflammation and transduces colchicine effects in macrophages. Ann Rheum Dis. 2014. doi: 10.1136/annrheumdis-2014-206074 [Epub ahead of print].
