BOSTON—During a session titled, Systems Biology of Lupus Nephritis at the 2014 ACR/ARHP Annual Meeting, Nov. 17, participants heard from a panel of experts about a way to identify major pathogenic cell populations and pathways that lead to lupus nephritis (LN) based on the use of a systems analysis of renal gene expression in mice and humans. The ultimate goal of such an analysis is twofold: to enhance the understanding of the mechanisms of kidney inflammation and fibrosis in LN patients and to help identify and test novel disease biomarkers for LN to better predict which patients will respond to therapy.
Anne Davidson, MBBS, investigator at the Feinstein Institute for Medical Research, Manhasset, N.Y., who opened the session, emphasized the need to better identify the disease process of LN in individual patients so that therapy can be targeted to interfere with the biological mechanism currently damaging the tissue in each patient.
Although she said that medical intervention has changed the course and improved outcomes of people with LN, predicting outcomes remains difficult because of the unpredictable disease course and response to therapy in each patient. “This heterogeneity is not adequately reflected in the current descriptive clinical and histological disease classification,” she said.
As such, she emphasized that current methods of assessing LN from kidney biopsies are insufficient to predict the response to therapy by each individual patient and who will progress to renal failure.
From Mice to Men: Shared Molecular Features of LN
In her talk, Dr. Davidson described the work she and her colleagues have done looking at gene expression in the kidneys of mice models of LN and comparing the data with human biopsy samples.
“Molecular analyses of kidneys from mouse models of lupus show a number of shared features, and there is considerable overlap with data from human renal biopsies,” she said.
Focusing largely on research she and her colleagues have done on progressive disease and remission in NZB/W mice, she highlighted a number of relevant physiologic pathways activated at progressive stages of nephritis, as well as during remission and relapse in mice, that overlap with data from renal biopsies in humans (see Table 1).
Findings from these studies, she said, “are helping identify new pathways that contribute to kidney damage that are targets for therapy and … new biomarkers that can be used to help individualize treatment.”
In Situ Adaptive Immunity

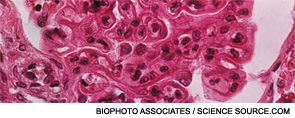
Marcus Clark, MD, chief, Section of Rheumatology, Gwen Knapp Center for Lupus and Immunology Research, the University of Chicago, spoke on in situ adaptive immunity in LN. Among the key points of his talk was the prognostic importance of tubulointerstitial inflammation at the time of biopsy, which is a better indicator than glomerular inflammation in predicting the risk of progression to renal failure, with increased risk of progression to renal failure in patients with moderate to severe tubulointerstitial inflammation.
Severe tubulointerstitial inflammation, he said, is associated with B cell selection in situ mediated by T-follicular helper cells, and the antibodies selected in situ often react with a molecule called vimentin, which is highly expressed in inflammatory infiltrates.
“High-titer serum antibodies to vimentin in the serum appear to be a specific biomarker of severe tubulointerstitial disease,” he said. “This would be the first biomarker in blood for a specific histologic manifestation of LN of such prognostic importance.”
TWEAK

Chaim Putterman, MD, chief, Division of Rheumatology, Albert Einstein College of Medicine and Montefiore Medical Center, Bronx, N.Y., spoke on the TNF-related weak inducer of apoptosis (TWEAK) molecule as a potential therapeutic target and biomarker for active LN. He presented data from a number of studies that show that the TNF-family member cytokine TWEAK, acting through the fibroblast growth factor-inducible 14 (Fn14), promotes inflammatory diseases by activating key cell types that drive pathology locally rather than by modifying adaptive immune responses.
He also highlighted data showing that inhibition of TWEAK signaling is effective in several experimental models of immune-mediated renal disease, including chronic graft-vs.-host (cGVH) disease, nephrotoxic serum nephritis and spontaneous LN in mice (i.e., MRL-lpr/lpr mouse strain).
Data show as well that TWEAK is up-regulated in kidneys of mice and patients with active LN and can be found in the urine of lupus patients with active nephritis. Although he said this does not necessarily mean that TWEAK is pathogenic or directly injurious to the kidney, the presence of TWEAK in the urine of individuals with active LN “suggest a possible role of urinary TWEAK as a biomarker either used alone or maybe as a part of a larger panel of molecules that are up-regulated during nephritis but that wouldn’t be up-regulated in kidneys without active inflammation or in kidneys with nephritis, but not from lupus.”
Based on these and other studies, Dr. Putterman said that a large, multinational, Phase II clinical trial called ATLAS is currently enrolling patients to formally look at the role of an anti-TWEAK antibody as an add-on to the standard of care for patients with LN (see https://clinicaltrials.gov/ct2/show/NCT01499355?term=ATLAS+and+lupus&rank=1).
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.


