BOSTON—The pathogenesis of psoriatic arthritis, its clinical manifestations and ways to diagnosis it, along with a rational approach to treatment, were all discussed during a session on Psoriatic Arthritis: Skin, Entheses and Joints at the ACR/ARHP Annual Meeting in Boston in November 2014.
Aim Higher: Treatment for Psoriasis
Kenneth B. Gordon, MD, professor of dermatology, Northwestern University, Feinberg School of Medicine, Chicago, opened the session with a discussion of current efforts to treat and improve treatment for psoriasis. Opening with a quote from John Updike, who described the humiliation of having psoriasis, Dr. Gordon emphasized the significant impact of this condition on patients’ lives in determining the goals of therapy.
For example, he said that people with psoriasis on both their hands are considered to have a mild case of psoriasis, but he emphasized the significant impact this can have on, for example, professional people who, by etiquette, need to shake hands with their clients. He cited young women with scalp psoriasis as another example of patients who are significantly affected by the disease.
Citing data showing that the No. 1 reason that patients no longer seek treatment for psoriasis is that they’ve given up trying to get sufficient treatment, he highlighted that the goals of treatment often differ between patient and physician and urged physicians to think of psoriasis in the context of the general health of patients. This includes not only improving the primary disease, but also looking at and treating co-morbid diseases (such as frequent depression and cardiovascular disease) and overall emotional and economic needs that can significantly affect patients. For example, he said that the economic impact of psoriasis can be particularly significant for lower income people, a high percentage of whom have severe disease.
As such, he recommends aggressive treatment for treating the skin disease (and not joint disease) in patients with psoriasis. Highlighting new information on the importance of achieving Psoriasis Area and Severity Index (PASI) of at least 90% reduction (PASI90) instead of the current standard measure of 75% reduction (PASI75) on improving the disease, he said that the PASI75 and PASI90 achieved with the current standard therapy with methotrexate is suboptimal.1,2
Other oral medications, such as apremilast, are similar to methotrexate in terms of PASI response, he said, but have a better tolerability that may be needed for some patients.
To provide more optimal treatment, he referred to new information on the pathogenesis of psoriasis that shows the importance of the IL-17 pathway in connecting the inflammatory response and clinical presentation of psoriasis.
Published phase II data on therapies that target IL-17, such as ixekizumab and brodalumab, he said, show better improvement than the currently available drugs to reduce PASI75, and particularly PASI90 and PASI100.3,4 He said these numbers suggest the possibility of clearing patients of psoriasis without the concern of significant side effects.
In the next few months, he expects FDA approval on secukinumab (300 mg) based on the one new therapy with published phase III data showing sustained and high PASI75 response rates.5 The study also shows improvement in PASI90 response, which is associated with greater improvements in quality of life, he said.
Over the past year, these new therapies that seek to attain higher response levels have been providing exciting possibilities for patients and the physicians who treat them to meet the goals of improving joints and, importantly, the significant impact of psoriasis on the skin.
Pathogenesis of Psoriatic Arthritis—Linked to Synovio-Entheseal Complex

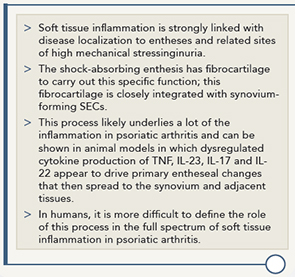
Dennis McGonagle, PhD, professor of investigative rheumatology, Section of Musculoskeletal Disease, Leeds Institute of Rheumatic & Musculoskeletal Medicine, St. James Hospital, University of Leeds, Leeds, West Yorkshire, England, walked participants through his research on the synovio-entheseal complex (SEC) that shows that SEC is key to understanding soft tissue inflammation in patients with psoriatic arthritis. Table 1 highlights key points of his research.
Of importance to rheumatologists, he said, is the need to recognize that soft tissue inflammation and bursitis may be due to SEC disease, and that early enthesitis-related pathology may manifest in the bursae or in entities like dacyliits.
Having this better understanding of the disease pathology, he said, will help clinicians diagnose the disease.
To further help clinicians understand SEC, he is building an educational resource on enthesis that can be accessed at http://enthesis.info/anatomy/synovio-entheseal_complex.html.
Clinical Manifestations & Rational Approach to Treatment

First focusing on the clinical manifestations of psoriatic arthritis, Christopher T. Ritchlin, MD, MPH, chief, Department of Allergy, Immunology & Rheumatology Division, director, Translational Immunology Research Center, University of Rochester Medical Center, Rochester, N.Y., emphasized the importance of differentiating true psoriasis from a number of other possible skin conditions that mimic it (e.g., atopic or contact dermatitis, tinea, onychomycosis, seborrheic dermatitis, psoriasiform lesions of SLE, cutaneous T cell lymphoma, acute generalized exanthematous pustulosis [AGEP] and keratoderma) and encouraged rheumatologists to refer patients to a dermatologist if they are in doubt.
Along with the skin, the key domains of psoriatic arthritis that need evaluation are the nails, peripheral arthritis, dactylitis, enthesitis and axial disease.
Echoing Dr. Gordon, he also emphasized the need to consider the number of comorbidities often seen in patients with psoriatic arthritis, including obesity, type II diabetes mellitus, hypertension, uveitis, inflammatory bowel disease, anxiety and depression, metabolic syndrome and increased risk of cardiovascular disease. All of these, he said, contribute to increased disability and decreased quality of life and life expectancy.
A better recognition of the many manifestations of psoriatic arthritis can help facilitate an earlier diagnosis and treatment, both of which are often delayed because of the varied presentation of psoriatic arthritis among individuals and the lack of a diagnostic biomarker.
Once diagnosis is made, the challenges of managing psoriatic arthritis arise, said Dr. Ritchlin, because of the dearth of evidence on the efficacy of traditional agents (e.g., methotrexate, azulfidine, cyclosporine, leflunomide), whether traditional agents slow radiographic progression, whether traditional agents are effective for axial disease, dactylitis or enthesopathy, and the multiple comorbidities of many patients.
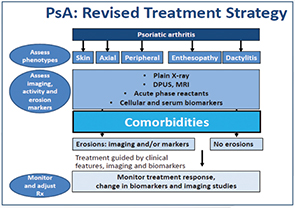
To help rheumatologists develop a comprehensive and feasible treatment plan, he proposed a treatment strategy guided by clinical features, imaging and biomarkers (see Figure 1). He also emphasized the importance of addressing comorbidities and collaborating with other medical specialists and primary care physicians to manage these conditions, as well as to recognize that certain agents to treat psoriatic arthritis may be contraindicated in patients with specific comorbidities.
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.
Second Chance
If you missed this session, Psoriatic Arthritis: Skin, Entheses and Joints, it’s not too late. Catch it on SessionSelect: http://acr.peachnewmedia.com/store/provider/provider09.php.
Key Evidence-Based Medicine References for Physicians
- Lowes MA, Suárez-Fariñas M, Krueger JG. Immunology of psoriasis. Ann Rev Immuno. 2014;32:227–255.
- Wendling D, Guillot X, Prati C. The IL-23/Th17 pathway in SpA: The Royal Road. Joint Bone Spine. 2014. Sep 19. pii: S1297-319X(14)00195-X. doi: 10.1016/j.jbspin.2014.08.003
- Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbiditis in patients with psoriatic arthritis: A comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63(12):1729–1735.
- Haroon M, Winchester R, Giles JT, et al. Certain class I HLA alleles and hapylotypes implicated in susceptibility play a role in determining specific features of psoriatic arthritis phenotype. Ann Rheum Dis. 2014 Sep 26. pii: annrheumdis-2014-205461. doi: 10.1136/annrheumdis-2014-205461.
References
- Revicki D, Chau D, Viswanathan HN, et al. 71st Annual Meeting of the American Academy of Dermatology 2013, abstract P6613.
- Reich K, Langley RG, Papp KA, et al. A 52-week trial comparing briakinumab with methotrexate in patients with psoriasis. N Engl J Med. 2011;365(17):1586–1596.
- Leonardi C, Matheson R, Zachariae C, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med. 2012;366(13):1190–1199.
- Papp KA, Leonardi C, Menter A, et al. Brodalumab, an anti-interleukin-17-receptor antibody for psoriasis. N Engl J Med. 2012;366(13):1181–1189.
- Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis—Results of two phase 3 trials. N Engl J Med. 2014;371:326–338.