BOSTON—In a session titled, New Regulatory T Cells, at the ACR/ARHP Annual Meeting in Boston in November 2014, Harvey Cantor, MD, chair of the Department of Cancer Immunology and AIDS, Dana-Farber Cancer Institute, Harvard Medical School, Boston, spoke about the way regulatory T cells (Treg) are changing the approach to understanding autoimmune diseases and, particularly, rheumatoid arthritis (RA).
Opening with a brief review of immunological self-tolerance, Dr. Cantor described two major T cell subsets that mediate regulatory activity—CD4 Treg and the relatively newly identified CD8 Treg—and recent work showing the critical role played by the expression of transcription factor Helios in maintaining the regulatory function of Treg. As a member of the Ikaros family of zinc finger transcription factors, Helios is specifically expressed by T cells and expressed at the earliest stages of T cell development, according to Dr. Cantor
The emerging important contribution by Helios to the development and function of regulatory T cells and subsequent effect on autoimmune disease was a major focus of his talk. Referring to the Helios of Greek mythology, the individual god who controlled the path of the sun and regulated the balance between earth and sun so earth didn’t get too hot or too cold, Dr. Cantor said the contribution of Helios to Treg and self-tolerance exerts an analogous regulating balance.
To describe this balancing influence of Helios, he discussed research showing how Helios maintains Treg function and stability/expansion during inflammation, and the potential for development of Treg-based therapies to treat rheumatoid arthritis (RA) and other autoimmune diseases.
Role of Helios in Autoimmunity
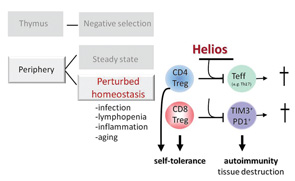
Based on their research to date, Dr. Cantor described a working model that he and his colleagues are using to test in mice what their data suggest regarding the role of Helios in the function of Treg and its effect on autoimmunity (see Figure 1).
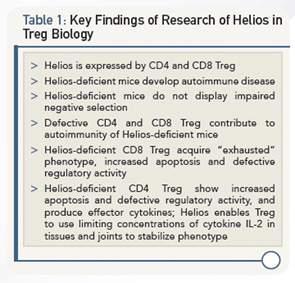
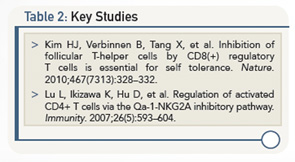
They are also beginning to use the model to look at people with autoimmune disease. A summary of the key findings of this research are shown in Table 1 and key studies in Table 2.
According to Dr. Cantor, the model describes the effect of Helios on T cell regulation (CD4 and CD8) and its effect on autoimmunity.
“After a change in homeostasis in the periphery, say after an infection, lymphopenia, inflammation or even aging,” he said, “the regulatory T cells in this environment are in a difficult position because of, in the case of CD4 Treg, an excess of inflammatory cytokines and less access to IL-2. Without the interception of Helios, these cells may die or become effector cells.”
The effect of Helios on CD8 Treg is similar. “Without the interception of Helios, these cells may undergo apoptosis,” he said.
In both situations, he said, these effects of Helios would result in enhanced levels of autoimmune tissue destruction.
Looking Ahead
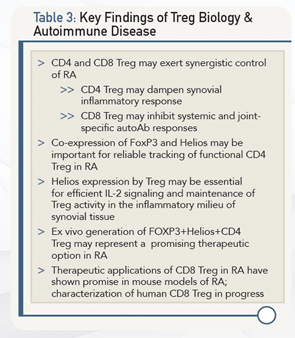
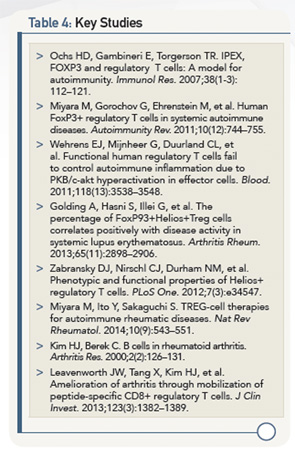
According to Dr. Cantor, further insight into both CD4 Treg and CD8 Treg, particularly as they relate to Helios, will pay off in terms of future ways to diagnose and treat RA. Table 3 lists key findings from current research that is leading toward this goal, and Table 4 lists key studies.
Although currently in its infancy, Treg-based therapy has the potential to help patients with RA and other autoimmune diseases. Critical to achieving this, Dr. Cantor said, is finding a way to expand Helios+ FoxP3+ regulatory T cells, cells that are potent suppressors of autoreactive CD4 T cells.
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.
Second Chance
If you missed this session, it’s not too late. Catch it on SessionSelect.