At the 2015 ACR/ARHP Annual Meeting, the ACR unveiled the 2015 Guideline for the Treatment of Rheumatoid Arthritis.
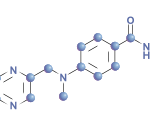
The introduction states: “Because there has been rapid accrual of evidence and new therapies, advancement of guideline development methodologies, and the need to broaden the scope of its 2012 RA recommendations, the ACR has developed a new 2015 RA pharmacologic treatment guideline. This guideline addresses six major topics: 1) use of traditional disease-modifying anti-rheumatic drugs (traditional/conventional DMARDs, herein referred to as DMARDs), biologic DMARDs (herein referred to as biologics), and tofacitinib, including tapering and discontinuing medications, and a treat-to-target approach; 2) use of glucocorticoids; 3) use of biologics and DMARDs in high-risk populations (i.e., those with hepatitis, congestive heart failure, malignancy, and serious infections); 4) use of vaccines in patients starting/receiving DMARDs or biologics; 5) screening for tuberculosis (TB) in the context of biologics or tofacitinib; and 6) laboratory monitoring for traditional DMARDs.”
According to the guideline authors, “This RA guideline should serve as a tool for clinicians and patients … for pharmacologic treatment decisions in commonly encountered clinical situations. These recommendations are not prescriptive, and the treatment decisions should be made by physicians and patients through a shared decision-making process, taking into account patients’ values, preferences and comorbidities. These recommendations should not be used to limit or deny access to therapies.”
Jasvinder Singh, MD, MPH, a rheumatologist at the University of Alabama who served as principal investigator for the guideline project, told members of the press, “We could not cover every possible clinical scenario in the guideline.” He also emphasized that the recommendations are not meant to be used for insurance purposes.
The guideline includes 74 recommendations: 23% are strong and 77% are conditional. It covers the use of traditional disease-modifying anti-rheumatic drugs (DMARDs), biologic agents, tofacitinib and glucocorticoids in early (<6 months) and established (≥6 months) RA.
Topping the list of recommendations for both early and established RA is the strong recommendation to, regardless of disease activity level, use a treat-to-target approach rather than a non-targeted approach.
In addition, it provides recommendations on tapering and discontinuing medications, and the use of biologic agents and DMARDs in patients with hepatitis, congestive heart failure, malignancy, and serious infections. The guideline addresses the use of vaccines in patients starting/receiving DMARDs or biologic agents, screening for tuberculosis in patients starting/receiving biologic agents or tofacitinib, and laboratory monitoring for traditional DMARDs.
For an executive summary of recommendations for patients with early RA, established RA and high-risk comorbidities, go to Supplementary Appendix 5.
Excerpted and adapted from:
Singh JA, Saag KG, Bridges SL Jr., et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol. 2015 Dec;67(12).