Further research in 2013 pointed to the role of two more genes—the Mediterranean familial fever gene, MEFV, and TLR4—suggesting that innate immune and bacterial sensing mechanisms are at work in Behçet’s.3
Diagnostic Criteria for Children
Dr. Ozen drew special attention to the challenge of diagnosing children. According to criteria written in 1990, diagnosis of Behçet’s in children requires oral ulcers along with two of these four criteria: uveitis or retinal vasculitis, genital ulcers, pustules and/or erythema nodosum and pathergy.
Case study: A 12-year-old boy, for example, presented to her with jugular venous thrombosis, with a history of a cardiac pacemaker, recurrent ulcers for two or three years, non-specific arthralgia and a maternal history of Behçet’s. Ophthalmology and pathergy tests were negative.
Finally, a stool system was positive for blood, and a colonoscopy found ulcers typical of Behçet’s.
“We had to treat it as such—but when you look back, he presented to us with only one criteria—the oral ulcers only,” she said.
She suggests a wider set of new criteria—the details of which she is not ready to widely disseminate—which she hopes are helpful with diagnosis and management, “so that we can diagnose them earlier and treat them earlier, because, really, the diagnosis [may] be challenging sometimes.”
Treatment
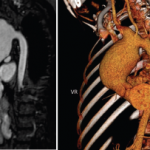
Treatment for Behçet’s is not well studied, but there are a few standards, Dr. Ozen said. She cautioned that patients with pulmonary aneurysms should not be given anticoagulants because of “a very significant risk of rupture.” But that is the only scenario in which anti-coagulants should not be used, she said.
A collaboration of three centers in France, Italy and Turkey studied thrombosis in pediatric Behçet’s and found that there was no consensus on whether to give anticoagulants in these patients, but Dr. Ozen said she does so “to be on the safe side.”4
The only evidence-established treatment is the immunosuppressant azathioprine for inflammatory eye disease, Dr. Ozen said, although she cautioned that azathioprine alone may not be enough.
Patients with pulmonary aneurysms should not be given anti-coagulants because of ‘a very significant risk of rupture.’ —Dr. Ozen
There is no evidence-based treatment for gastrointestinal involvement, but sulfasalazine, steroids, azathioprine and anti-tumor necrosis factor (anti-TNF) medications are recommended. First-line treatment for oral and genital ulcers is topical, she said. The anti-gout agent, colchicine, is recommended for nodular lesions.
There are no firm data for central nervous system involvement and vascular disease, she said, but steroids, cyclophosphamide, azathioprine, interferon and anti-TNFs have been recommended, “depending on the extent of the involvement.”