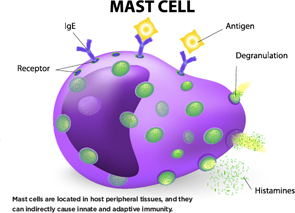
Mast cells are located in host peripheral tissues, and they can indirectly cause innate and adaptive immunity.
Designua/shutterstock.com
SAN FRANCISCO—What factors help determine whether or not inflammation resolves, leading to healing, or becomes chronic, leading to disease and tissue destruction?
A number of important cells, including toll-like receptors, mast cells, anti-citrullinated protein antibodies, complement and interferon, all play their own role in this process. By understanding how they act in innate and adaptive immunity and set off the disease process, rheumatologists may one day have more effective therapies to stop joint damage before it starts.
On Nov. 7, researchers at the 2015 ACR/ARHP Annual Meeting discussed the role some of these cells play in such diseases as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
Toll-Like Receptors, Mast Cells & ACPAs
Mast cells are best known for their role in allergies, said Rene E. M. Toes, PhD, head of the Rheumatology Laboratory at Leiden University Medical Center in The Netherlands. After an antigen enters the bloodstream, there is mast cell degranulation and inflammatory mediators are released, he said. This can lead to life-threatening reactions in humans.
Mast cells are located in host peripheral tissues, and they can indirectly cause innate and adaptive immunity. They’re found in inflamed synovial tissue in both RA and osteoarthritis. In one study published in Arthritis & Rheumatology in 2015, the number of mast cells found in OA synovium went up along with higher Kellgren and Lawrence scores, measures of disease severity, he said.1
In RA, mast cells are mostly found in the joint sublining. In spondyloarthritis, they are in the synovial tissue.
“Mast cells express many pattern recognition receptors,” said Dr. Toes. “Toll-like receptors are among these. Are human mast cells activated through toll-like receptors? If so, which ones?” Mast cells respond to toll-like receptor ligands with the production of IL-8, he noted.
Both cultured and synovial mast cells express the receptor FCγRIIA.2 Mast cells are activated by immune complexes in an FCγRIIA-dependent fashion. Combined toll-like receptors and FCγR triggering induces synergy in cytokine production, Dr. Toes said.
Can mast cells be activated by anti-citrullinated protein antibody (ACPA) immune complexes? “ACPA recognizes many different citrullinated proteins. In RA, ACPAs are important markers of disease development,” he said. ACPA-positive RA patients have higher levels of immunoglobulin-G (IgG). Mast cells respond to ACPA, and endogenous toll-like receptor ligands enhance mast cell activation by ACPA.
‘Why do they have lupus? Because they can’t clear complement. … This points to the idea that if you can’t clear debris, there is a problem.’ —John P. Atkinson, MD
In addition, mast cells often co-localize with CD4 and T cells, and they can also process and present protein antigens. Mast cells specifically enhance Th17 responses. And in activated mast cells, IL-17 T cell response is enhanced, he said.

