Hand and digit pain are common presenting symptoms to primary care physicians, rheumatologists, physiatrists and neurologists. There are many causes, but quality and location of the pain can be important clues to the diagnosis. Glomus tumors, neurovascular hamartomas of the glomus body, are an uncommon cause of hand pain.
The glomus unit itself is a neuromyoarterial apparatus that regulates skin temperature as an arteriovenous shunt. The glomus body is in the highest concentration in the subungual reticular dermis of the nail bed, where 75% of these lesions commonly occur.1 Other, less common, sites include the palm, wrist, forearm and foot. The symptomatic triad of paroxysmal night pain, cold sensitivity and acute point tenderness is often used to diagnose a glomus tumor. Occasionally, a pink or bluish nodule can be seen beneath the nail bed. However, affected patients often seek medical attention before the symptoms are fully developed and before the mass itself can be seen or palpated.
The differential diagnosis of nocturnal or rest hand pain should include glomus tumor (see Table 1), a condition that, although rare, may be confirmed promptly at point of care with clinical strategies alone (Case 1) and with supplemental imaging (Cases 2 & 3).
Case 1
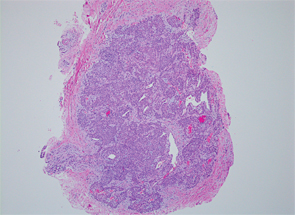
Figure 1: A hematoxylin and eosin stain showing abundant polyhedral glomus tumor cells—seen as rounded uniform epithelioid cells with granular cytoplasm. Courtesy of Dr. Savita Kulkarni, Humber River Hospital, Toronto
Biophoto Associates/sCIENCESOURCE.com
A 33-year-old female lawyer presented for the evaluation of hand pain with a two-year history of aching, tenderness and throbbing of the third digit of her left hand. Throbbing was reported to be worse at night and when exposed to colder temperatures. A night splint gave her no relief. Tinel’s sign was absent, Phalen’s test was negative, and the patient showed no clinical synovitis or tenosynovitis. The examination revealed an acutely tender 2×3 mm bluish splinter-like lesion under the nail, near the nail plate of the symptomatic third digit. Cold sensitivity was confirmed clinically (discussed below). Electrodiagnostic studies were normal. Based on the history and reproducible clinical findings, the surgeon agreed with the referral diagnosis of a glomus tumor.
The patient underwent a successful surgical excision of the tumor (see Figure 1).
The symptomatic triad of paroxysmal night pain, cold sensitivity & acute point tenderness is often used to diagnose a glomus tumor.
Case 2
A 46-year-old medical administrative assistant with psoriasis presented with a 12-year history of pain in the fourth right digit. She reported worse pain at night and when exposed to cold. The nail bed showed some discoloration and acute point tenderness at the site (see Figure 2). There was no distal IP joint tenderness or swelling and no psoriatic nail changes. An X-ray revealed an erosion of the ulnar portion of the distal phalanx, under the site of discoloration (see Figure 3).
Table 1. Differential Diagnosis of Nocturnal Hand Pain
- Neuropathic Cervical Radiculopathy Thoracic Outlet Syndrome Cubital Tunnel Syndrome Hypothenar Hammer Syndrome Carpal Tunnel Syndrome Painful Neuropathies
- Musculoskeletal De Quervain’s Tenosynovitis Trapezium/Metacarpal Osteoarthritis Inflammatory Arthropathies Crystal Arthropathies
- Chronic Infection Osteomyelitis Sarcoidosis
- Neoplastic Glomus Tumor Acrometastases Neuroma Subungual Melanoma
Point-of-care ultrasound (POCUS) study allowed the detection of a round-shaped 5 mm lesion under the nail bed of the fourth digit, where there was discontinuity of the distal phalanx cortex and an intense color Doppler signal consistent with a focal vascular lesion (see Figure 4).