Hand and digit pain are common presenting symptoms to primary care physicians, rheumatologists, physiatrists and neurologists. There are many causes, but quality and location of the pain can be important clues to the diagnosis. Glomus tumors, neurovascular hamartomas of the glomus body, are an uncommon cause of hand pain.
The glomus unit itself is a neuromyoarterial apparatus that regulates skin temperature as an arteriovenous shunt. The glomus body is in the highest concentration in the subungual reticular dermis of the nail bed, where 75% of these lesions commonly occur.1 Other, less common, sites include the palm, wrist, forearm and foot. The symptomatic triad of paroxysmal night pain, cold sensitivity and acute point tenderness is often used to diagnose a glomus tumor. Occasionally, a pink or bluish nodule can be seen beneath the nail bed. However, affected patients often seek medical attention before the symptoms are fully developed and before the mass itself can be seen or palpated.
The differential diagnosis of nocturnal or rest hand pain should include glomus tumor (see Table 1), a condition that, although rare, may be confirmed promptly at point of care with clinical strategies alone (Case 1) and with supplemental imaging (Cases 2 & 3).
Case 1
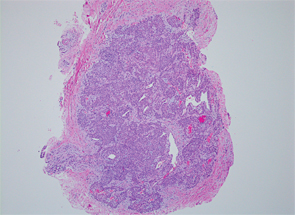
Figure 1: A hematoxylin and eosin stain showing abundant polyhedral glomus tumor cells—seen as rounded uniform epithelioid cells with granular cytoplasm. Courtesy of Dr. Savita Kulkarni, Humber River Hospital, Toronto
Biophoto Associates/sCIENCESOURCE.com
A 33-year-old female lawyer presented for the evaluation of hand pain with a two-year history of aching, tenderness and throbbing of the third digit of her left hand. Throbbing was reported to be worse at night and when exposed to colder temperatures. A night splint gave her no relief. Tinel’s sign was absent, Phalen’s test was negative, and the patient showed no clinical synovitis or tenosynovitis. The examination revealed an acutely tender 2×3 mm bluish splinter-like lesion under the nail, near the nail plate of the symptomatic third digit. Cold sensitivity was confirmed clinically (discussed below). Electrodiagnostic studies were normal. Based on the history and reproducible clinical findings, the surgeon agreed with the referral diagnosis of a glomus tumor.
The patient underwent a successful surgical excision of the tumor (see Figure 1).
The symptomatic triad of paroxysmal night pain, cold sensitivity & acute point tenderness is often used to diagnose a glomus tumor.
Case 2
A 46-year-old medical administrative assistant with psoriasis presented with a 12-year history of pain in the fourth right digit. She reported worse pain at night and when exposed to cold. The nail bed showed some discoloration and acute point tenderness at the site (see Figure 2). There was no distal IP joint tenderness or swelling and no psoriatic nail changes. An X-ray revealed an erosion of the ulnar portion of the distal phalanx, under the site of discoloration (see Figure 3).
Table 1. Differential Diagnosis of Nocturnal Hand Pain
- Neuropathic Cervical Radiculopathy Thoracic Outlet Syndrome Cubital Tunnel Syndrome Hypothenar Hammer Syndrome Carpal Tunnel Syndrome Painful Neuropathies
- Musculoskeletal De Quervain’s Tenosynovitis Trapezium/Metacarpal Osteoarthritis Inflammatory Arthropathies Crystal Arthropathies
- Chronic Infection Osteomyelitis Sarcoidosis
- Neoplastic Glomus Tumor Acrometastases Neuroma Subungual Melanoma
Point-of-care ultrasound (POCUS) study allowed the detection of a round-shaped 5 mm lesion under the nail bed of the fourth digit, where there was discontinuity of the distal phalanx cortex and an intense color Doppler signal consistent with a focal vascular lesion (see Figure 4).
At surgery, a glomus tumor was excised.
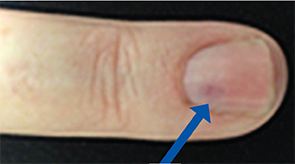
Figure 2: The nail bed shows some discoloration.
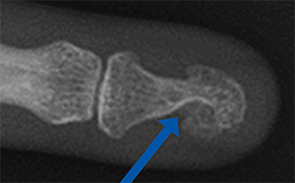
Figure 3: Erosion is seen at the distal phalanx.
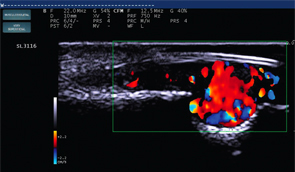
Figure 4: Color Doppler at the erosion site displays a 5 mm vascular lesion.
Case 3
A 33-year-old office manager presented with a two-year history of pain in the left hand and was referred for evaluation for possible median nerve entrapment at the wrist.
Electrodiagnostic studies and ultrasound of the carpal tunnel were normal. Her symptoms were most intense at the fourth fingernail bed, where she displayed acute tenderness to palpation and to pressure from the ultrasound probe. Discoloration under the nail (see Figure 5,) was apparent.
POCUS was performed at the symptomatic site, using a high-resolution 22 MHz ultrasound transducer. For the ultrasound assessment of superficial structures, such as the nail bed, a very high-frequency probe is required. (Note: In cases 2 and 3, a 22 MHz linear probe was used [see Figure 6]). A vascular malformation consistent with a 2 mm glomus tumor was suspected (see Figure 7). The ultrasound study guided the follow-up MRI examination, confirming an isolated glomus tumor (see Figure 8). The lesion was surgically excised.

Figure 5: A splinter-shaped bluish discoloration under the nail bed.
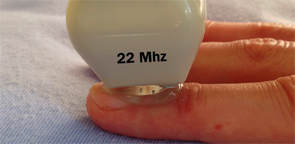
Figure 6: A high-frequency linear ultrasound probe (22 MHz) allows for very high-resolution imaging of superficial structures.
1 Year Later
All three patients report they are pain free one year after excisional therapy performed by a hand surgeon.
About Glomus Tumors
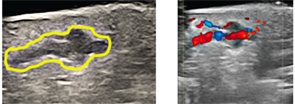
Figure 7: An irregular heterogeneous mass under nail on B Mode and a highly vascular discrete lesion on color Doppler.
Glomus tumors normally occur in tissues rich in glomus bodies: temperature- and pressure-sensitive receptors present in the stratum reticularis of the dermis. They represent 1–4% of all soft-tissue hand tumors. Roughly 70% of single tumors occur in patients younger than 30, and multiple tumors most often occur in patients between ages 15 and 20.2,3 Tumors can appear anywhere that glomoid cell types occur, and subungual glomus tumors are more common among women.2,4,5
As hamartomas, glomus tumors are formed from a hyperplasia of normal tissue.2,6 There are abundant polyhedral glomus tumor cells, seen as rounded uniform epithelioid cells with granular cytoplasm (see Figure 1). Staining with actin highlights smooth muscle surrounding vascular channels and neural elements (Figure 9).
Early diagnosis can prevent prolonged morbidity and extensive investigations. Despite effective clinical and imaging diagnostic methods, patients can experience delays in diagnosis of months or even years, as seen with the three cases detailed above.
The three most common indicators of glomus tumors are intense paroxysmal pain, point tenderness and cold sensitivity.2,3,7
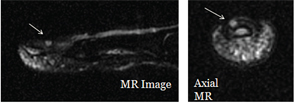
Figure 8: POCUS is used to guide an MRI study of a nail bed.
Three common clinical methods of diagnosis can be used to effectively distinguish glomus tumors from other similarly sized or located masses. Hildreth’s sign refers to the temporary relief of pain at the site of the lesion by inducing ischemia with a pressure cuff.8 Love’s pin test, in which a pinhead is used to apply pressure to the site of the tumor, should produce intense pain.9 A cold sensitivity test, which is conducted by applying cold water, an ice cube or any other material that causes a drop in temperature at the site of the lesion, should produce intense pain.10
Imaging is often used to verify the diagnosis prior to surgical intervention. Standard radiographs are typically normal, but erosion of the bone can occur in some cases (as seen in Case 2).11 MRI can be most effectively used for confirming the diagnosis and the tumor’s location.10,12 MR imaging can produce false-negative results in 10% of cases. Resolution is a limiting factor, allowing small lesions to be undetected.12
Ultrasound can detect tumors as small as 2 mm in diameter, gives better visualization of tumors when compared with standard radiology techniques, and is less expensive and time consuming than MRI. Color or power Doppler ultrasound (used on Patients 2 and 3) provides enhanced vascular detail when compared with grey-scale methods.3,5,13,14
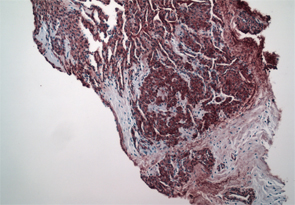
Figure 9: Smooth muscle actin immunostain shows smooth muscle surrounding vascular channels and neural elements. Courtesy of David Chercover, MD, Lions Gate Hospital, North Vancouver, B.C.
The standard course of treatment for a glomus tumor is surgical excision. Multiple tumors are reported. Recurrences are uncommon and are generally due to incomplete excision.12
Digital glomus tumors are small, rare causes of hand pain. Their small size and low prevalence make an early diagnosis difficult. As in our cases, no predisposing or risk factors are known, although the condition is three times more common in women. When faced with symptoms of paroxysmal pain, cold sensitivity and acute tenderness, physicians have clinical strategies that can be employed to identify glomus tumors with greater certainty.
Radiographic pressure erosions are late to appear, and MRI is limited by poor resolution for these small lesions. Point-of-care ultrasound is an ideal modality to confirm the presence of a hypoechoic, discrete, well-defined vascular lesion and limit the duration of preoperative morbidity. Access to high-resolution point-of-care ultrasound is suggested as a method of rapid, sensitive, inexpensive confirmation of diagnosis at peripheral sites common for glomus tumor.
 Abraham Chaiton, MD, MSc, FRCPC, RhMSUS, is a graduate of the University of Toronto, where he is an assistant professor in rheumatology. He trained in clinical epidemiology at McMaster University, Hamilton, Ontario, Canada, and as a neuromuscular fellow at Toronto General Hospital. He is a member of the Neurodiagnostic Lab at Humber River Hospital, a founding member and executive staff of the Canadian Rheumatology Ultrasound Society, a past member of the ACR Ultrasound Certification Committee, a member of AANEM Ultrasound Education Committee, active staff at Sunnybrook and Humber River Hospitals, Toronto, and associate staff at Lions Gate Hospital in North Vancouver, B.C. His clinical interests include biologic therapies, myositis, focal nerve entrapments, ultrasound-guided interventions and teaching of POCUS to students and clinicians.
Abraham Chaiton, MD, MSc, FRCPC, RhMSUS, is a graduate of the University of Toronto, where he is an assistant professor in rheumatology. He trained in clinical epidemiology at McMaster University, Hamilton, Ontario, Canada, and as a neuromuscular fellow at Toronto General Hospital. He is a member of the Neurodiagnostic Lab at Humber River Hospital, a founding member and executive staff of the Canadian Rheumatology Ultrasound Society, a past member of the ACR Ultrasound Certification Committee, a member of AANEM Ultrasound Education Committee, active staff at Sunnybrook and Humber River Hospitals, Toronto, and associate staff at Lions Gate Hospital in North Vancouver, B.C. His clinical interests include biologic therapies, myositis, focal nerve entrapments, ultrasound-guided interventions and teaching of POCUS to students and clinicians.
 Maggie Larché, MBChB, MRCP, PhD, is an associate professor in the Divisions of Rheumatology and Clinical Immunology and Allergy in the Department of Medicine & Pediatrics at McMaster University and staff Physician at St. Joseph’s Hospital in Hamilton, Ontario, Canada. Following a PhD from Imperial College, London, she trained in rheumatology in London, U.K. She is a founding member and past president of the Canadian Rheumatology Ultrasound Society and chair of the Hamilton Scleroderma Group. Her major clinical interest is in scleroderma and early inflammatory arthritis, with research interests in cellular biomarkers and ultrasonographic and MR imaging in inflammatory arthritis.
Maggie Larché, MBChB, MRCP, PhD, is an associate professor in the Divisions of Rheumatology and Clinical Immunology and Allergy in the Department of Medicine & Pediatrics at McMaster University and staff Physician at St. Joseph’s Hospital in Hamilton, Ontario, Canada. Following a PhD from Imperial College, London, she trained in rheumatology in London, U.K. She is a founding member and past president of the Canadian Rheumatology Ultrasound Society and chair of the Hamilton Scleroderma Group. Her major clinical interest is in scleroderma and early inflammatory arthritis, with research interests in cellular biomarkers and ultrasonographic and MR imaging in inflammatory arthritis.
References
- Lee W, Kwon SB, Cho SH, et al. Glomus tumor of the hand. Arch Plast Surg. 2015 May;42(3):295–301.
- Gombos Z, Zang PJ. Glomus tumor. Arch Pathol Lab Med. 2008 Sep;132(9):1448–1452.
- Nazerani S, Motamedi MKM, Keramati MR. Diagnosis and management of glomus tumors of the hand. Tech Hand Up Extrem Surg. 2010 Mar;14(1):8–13.
- Motandon C, Costa JD, Dias LA, et al. Tumores glomicos subunguearis. Radiol Bras. 2009;42(6):371–374.
- Marchadier A, Cohen M, Legre R. [Subungual glomus tumors of the fingers; ultrasound diagnosis.] Chir Main. 2006 Feb;25(1):16–21.
- Tuncali D, Yilmaz AC, Terzioglu A, Aslan G. Multiple occurrences of different histologic types of glomus tumor. J Hand Surg Am. 2005 Jan;30(1):161–164.
- McDermott EM, Weiss APC. Glomus tumors. J Hand Surg Am. 2006 Oct;31(8):1397–1400.
- Hildreth DH. The ischemic test for glomus tumor: A new diagnostic test. Review of Surg. 1970 Mar–Apr;27(2):147–148.
- Love JG, Glomus tumors: Diagnostic and treatment. Proc Staff Meet, Mayo Clinic. 1944;19:113–116.
- Netscher DT, Aburto J, Koepplinger M. Subungual glomus tum0or. J Hand Surg Am. 2012 Apr;37(4):821–823.
- Kim DH. Glomus tumor of the finger tip and MRI appearance. Iowa Orthopaedic J. 1999;19:136.
- Tang CYK, Tipoe T, Fung B. Where is the lesion? Glomus tumours of the hand. Arch Plast Surg. 2013 Sep;40(5):492–495.
- Chen SHT, Chen YL, Cheng MH, et al. The use of ultrasonography in preoperative localization of digital glomus tumors. Plast Recon Surg. 2003 Jul;112(1):115–119, discussion 120.
- Espinoze-Gutierrez A, Izaquirre A, Baena-Ocampo L, et al. Glomus tumor. J Rheumatol. 2009 Jun;36(6):1343–1344.
Disclosure
Drs. Chaiton and Larché have both received honoraria related to teaching ultrasonography courses through the Canadian Rheumatology Ultrasound Society from 2010–present.