Denied claims represent unpaid services, or lost or delayed revenue. Avoiding claims denials is the responsibility of everyone in a practice. Any deficiency on a focused strategy for denials management will have unfavorable resolutions to denials or lead to writing off the service without payment. With the changing landscape in practice management, the best route may not be to continue doing things the same way, with no change in outcomes. Quality improvement is crucial to actively achieve successful claims resolution.
Millions of claims are submitted to payers every day for services provided to patients. The majority of those claims are adjudicated immediately and processed with payment for the full contracted amount, but a notable minority is rejected and unpaid. The American Medical Association reported that between 1.38% and 5.07% of claims are denied by insurers on the first submission. Even a good performing practice can experience a denial rate of approximately 5%. This has a significant and avoidable impact on administrative resources and cost to the medical practice, and employees must spend a lot of time managing and, ideally, resolving claims denials.
Developing and optimizing proven strategies that result in claims payments are crucial. The four steps in effective denial management—identify, manage, monitor and prevent—must be understood, and practices must be vigilant in performing these steps to efficiently optimize their revenue.
Step 1: Identify
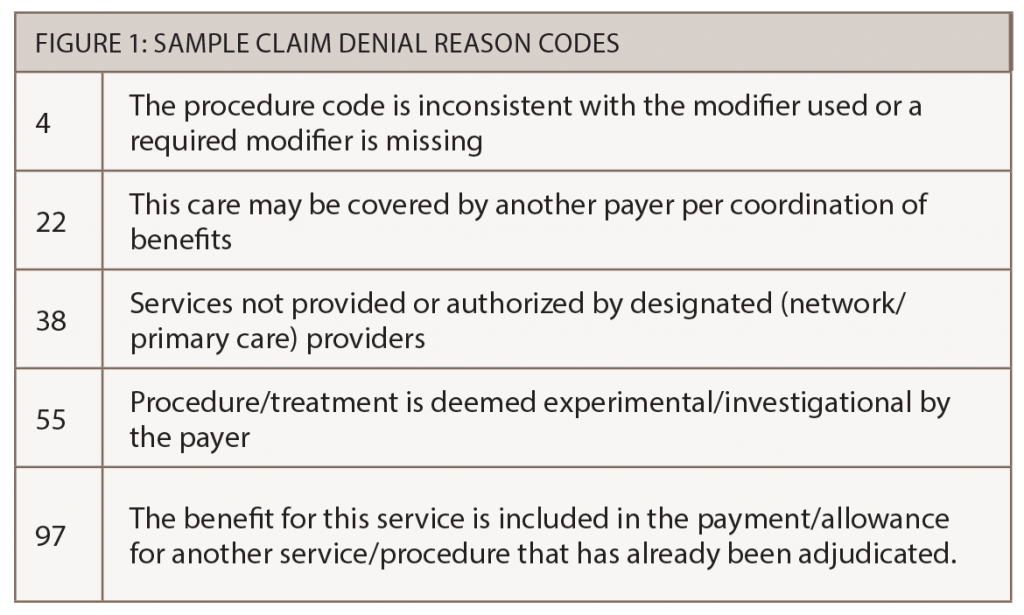
The first step in a successful claims resolution approach is to identify the reason a claim has been denied. All payers will explain a denial on their claims remittance or explanation of benefits (EOB). These denial codes are applied at the line item for each Current Procedural Terminology (CPT) code. Use these codes as clues for how to submit a corrected claim or for a successful appeal.
The codes are typically in alpha-numeric form, so staff will need to map the payer’s denial code to the description of the reason. Many of the codes are cryptic, for example, a denial code may read: Claim/service lacks information which is needed for adjudication. The payer denied the claim because additional information is needed, but what information is lacking? This will require staff to go hunting for additional information critical to reprocess and get the claim paid.
The denial reason codes also have a two-letter alpha code (typically preceding the reason codes) that indicates who is responsible to pay the denied amount. These alpha codes include “PR” to indicate patient responsibility and “CO” for contractual obligation—meaning the participating physician is contractually obligated to accept the denial.
Despite the challenges staff may encounter with denial codes, identifying the type of denial for any claim is the first step in a resolution. Not understanding a payer’s denial codes or not addressing what the codes convey may cause the claim to be denied a second time.