Denied claims represent unpaid services, or lost or delayed revenue. Avoiding claims denials is the responsibility of everyone in a practice. Any deficiency on a focused strategy for denials management will have unfavorable resolutions to denials or lead to writing off the service without payment. With the changing landscape in practice management, the best route may not be to continue doing things the same way, with no change in outcomes. Quality improvement is crucial to actively achieve successful claims resolution.
Millions of claims are submitted to payers every day for services provided to patients. The majority of those claims are adjudicated immediately and processed with payment for the full contracted amount, but a notable minority is rejected and unpaid. The American Medical Association reported that between 1.38% and 5.07% of claims are denied by insurers on the first submission. Even a good performing practice can experience a denial rate of approximately 5%. This has a significant and avoidable impact on administrative resources and cost to the medical practice, and employees must spend a lot of time managing and, ideally, resolving claims denials.
Developing and optimizing proven strategies that result in claims payments are crucial. The four steps in effective denial management—identify, manage, monitor and prevent—must be understood, and practices must be vigilant in performing these steps to efficiently optimize their revenue.
Step 1: Identify
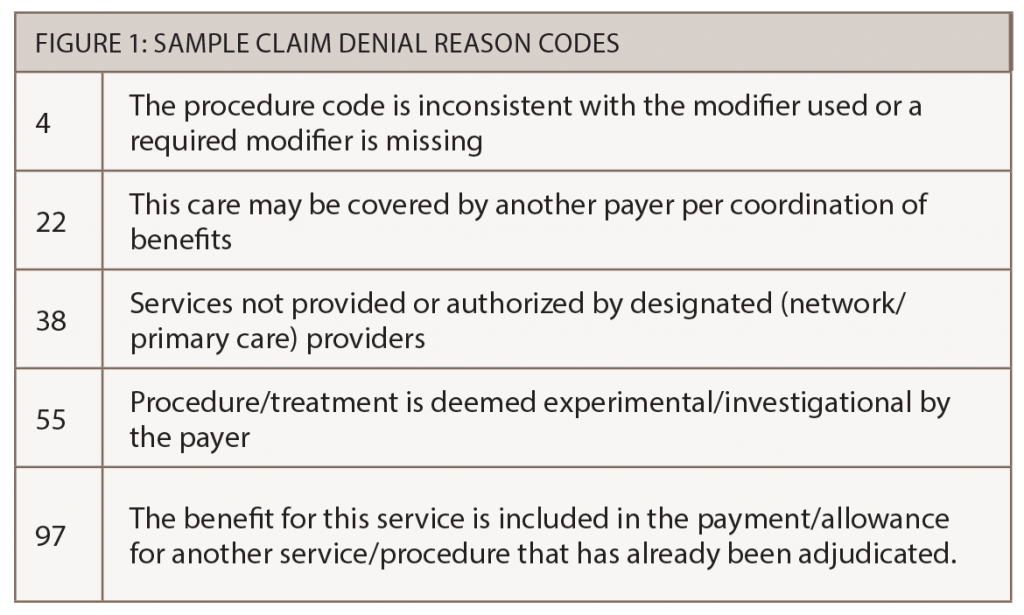
The first step in a successful claims resolution approach is to identify the reason a claim has been denied. All payers will explain a denial on their claims remittance or explanation of benefits (EOB). These denial codes are applied at the line item for each Current Procedural Terminology (CPT) code. Use these codes as clues for how to submit a corrected claim or for a successful appeal.
The codes are typically in alpha-numeric form, so staff will need to map the payer’s denial code to the description of the reason. Many of the codes are cryptic, for example, a denial code may read: Claim/service lacks information which is needed for adjudication. The payer denied the claim because additional information is needed, but what information is lacking? This will require staff to go hunting for additional information critical to reprocess and get the claim paid.
The denial reason codes also have a two-letter alpha code (typically preceding the reason codes) that indicates who is responsible to pay the denied amount. These alpha codes include “PR” to indicate patient responsibility and “CO” for contractual obligation—meaning the participating physician is contractually obligated to accept the denial.
Despite the challenges staff may encounter with denial codes, identifying the type of denial for any claim is the first step in a resolution. Not understanding a payer’s denial codes or not addressing what the codes convey may cause the claim to be denied a second time.
Step 2: Manage
Receiving a denial for a service unavoidably kicks off a series of tasks. Create a standard denials resolution workflow. Once the denial is identified, whether manually or automatically, an action plan to resolve and refile the claim for reprocessing must be executed. The following actions focus the work of denial management:
- Route the denial: Instead of printing, copying and filing each denied transaction, use automation to route denied claims directly into work lists. These lists should reflect the natural patterns of the revenue cycle. For example, route all coding-related denials to coders or providers. Sending a coding-related denial to the scheduler or front desk staff will only slow the process of handling the denial.
- Sort the work: Whether specific staff work denials as a component of their job or as their exclusive focus, make sure they have the technology and training to effectively do so. A structured, organized workflow—whether automated or manual—is critical. Staff can streamline the work by working denials based on category. For example, within an insurer category, work all denials related to a credentialing issue for a particular provider.
- Create a workflow: Create a standard workflow for each type of denial. Don’t attack the denial problem without a strategy for how to review and respond. Staff will comply with the process better if there is a carefully designed and monitored protocol. Identify your practice’s most common reasons for denials, such as medical necessity. Record the most frequent denial codes associated with that denial. For example, the diagnosis is inconsistent with the procedure. Develop a step-by-step action plan for staff to follow when managing one of those denials. Include even the most basic steps—check online claims status, then review the date of service and office note. With standard protocols, practices can achieve better performance throughout the denial management process. Hold staff accountable for their denial management tasks and accomplishments.
- Use a checklist: Effective denial management relies on many small actions carried out consistently and avoiding certain common mistakes that cause denials to linger and, in some cases, end up as uncollectable bad debt.
- Don’t delay. After a problem is identified, begin working on a resolution immediately.
- Avoid automatic rebilling because this tends to produce a significant number of duplicate claims and duplicate denials.
- Pick your battles. If research reveals the claim was filed incorrectly, correct it and resubmit it.
- Build the case for an appeal or resubmission by learning the payer’s requirements for resubmitting or appealing claims that may have been denied incorrectly.
Step 3: Monitor
The development of an effective denial management program takes more than just assigning a staff member to work denials and resubmit claims; the process must be monitored. To monitor the work of denial management, first maintain a log of denials by date received, type of denial and date appealed to ensure the denial management processes are effective. Second, audit the work of staff by selecting a sample of resubmissions and/or appeals. Evaluate the steps taken for the appeal, the timeliness of appeal and the strength of the case submitted to the payer. Third, make sure staff have the tools, technology and resources to get the job done.
Monitoring also must be conducted at the payer level to gain a better understanding of each payer’s claim denial system. While unpleasant to receive, claim denials, particularly the information about the type, number and source of the denial, are invaluable business data for a practice.
Step 4: Prevent
Armed with data regarding denials, the next step is to promote a prevention campaign. Managing a denial prevention program at the practice level is a natural step in running an efficient practice; developing a cross-functional approach prevents the common problem of one team fixing an issue, while another team corrects the issue. Teams working in parallel on the same problem may end up working at cross purposes, duplicating the work of others or failing to root out the problem altogether. Categories of denials that are prime targets for your denial prevention program include registration, coding, authorizations and medical necessity.
- Registration is the first area to review for claims denials. Determine whether the issue was the patient’s insurance coverage or benefits eligibility, or a combination of both. Produce a feedback method from staff regarding these denials, and offer additional training to resolve any problems identified.
- Coding can cause a huge problem due to the complexity of procedural or diagnosis coding. The key to solving coding-related denials is seizing the opportunity at the initial determination of the code, not after the fact. Identify common services, and gain expert advice on how to correctly code them. Preventing coding-related denials means providing physicians and staff with excellent training about appropriate code selection and documentation.
- There’s only one solution to avoiding denials based on lack of authorization, and it is simple: Always secure the required authorizations. It is tedious, but creates a process for staff to follow to ensure every prior authorization is captured for every service that requires one. Start by instituting a system to automatically query appointments for the prior authorization status of all scheduled services. Additionally, alert staff to investigate prior authorization requirements for all in-office services ordered on the spot.
- It’s frustrating for physicians to receive denials when the payer claims the diagnosis provided does not support the need for the service. There are options to respond to—and even reverse some of—these denials. To develop internal knowledge among providers and staff, gather all of your insurers’ policies regarding medical necessity. Organize the policies by procedure or diagnosis and set the electronic health record to provide alerts for services an insurer has deemed not medically necessary or those services that have special requirements for medical necessity. Appeal any denials based on necessity by attaching your documentation of the patient visit, as well as any relevant, current medical literature in support of that service’s efficacy.
Managing denials is costly in terms of time and money, and establishing an effective denial prevention program is crucial to the long-term success of the revenue cycle. Staff can be educated to streamline the practice workflow, improve internal processes and get reimbursed in a timely manner for services provided.
For questions or training on coding, billing and denials management, contact the ACR practice management department at [email protected].