 Gout is one of the most common inflammatory arthritis diseases, affecting 8.3 million adults in the U.S.1 It’s also one of the most preventable and treatable diseases, but only 32–58% of patients receive adequate gout treatment, indicating significant room for improvement of care.2
Gout is one of the most common inflammatory arthritis diseases, affecting 8.3 million adults in the U.S.1 It’s also one of the most preventable and treatable diseases, but only 32–58% of patients receive adequate gout treatment, indicating significant room for improvement of care.2
For this reason, the ACR supported a group that developed several electronic clinical quality measures (eCQMs) that aim to close this gap. These measures give rheumatologists the chance to measure their performance in key areas of gout care, including gout care management, management of urate-lowering therapy, management of patients on urate-lowering therapy, serum urate monitoring and management, allopurinol-specific considerations and gout flare prophylaxis.
“These quality measures are shining a light on gout to show the quality of care being provide to patients with gout and how patients are doing to help us improve patient outcomes,” says John FitzGerald, MD, PhD, interim chief of the division of rheumatology at Ronald Reagan UCLA Medical Center, Los Angeles. As a leader in gout research, Dr. FitzGerald led the ACR group’s work to shape these eCQMs and coauthored a paper outlining the development of these measures.2
Clinical Takeaways
To support rheumatologists and their colleagues in improving gout care management, Dr. FitzGerald outlines five practice takeaways from the eCQMs.
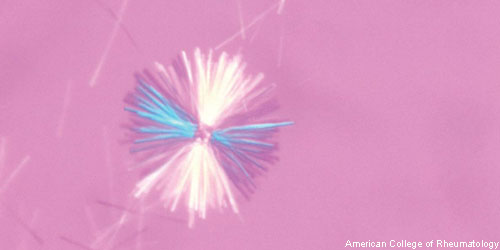
1. Identify gout patients with hyperuricemia in need of urate-lowering therapy: The first step in managing gout is to identify gout patients with hyperuricemia who require urate-lowering therapy, he says. According to the eQCMs, if a patient with gout has a serum urate (sUA) level greater than 6 mg/dL and has tophus/tophi development of two or more attacks per year, then urate-lowering therapy should be prescribed. This therapy will improve sUA levels, decrease the risk for recurrent attacks and reduce tophus deposition.2
2. Know the treat-to-target threshold for urate levels: Any patient with active gout on urate-lowering therapy should have their serum urate level checked at least once annually—at a minimum and regardless of disease activity. These patients should not have a sUA level above 6.8, according to the eQCMs. For patients being managed for active gout, the ACR recommended treatment target remains less than six, and less than five for patients with severe gout.
However, quality measures are meant to define a minimum threshold for all patients. Through this measure, a patient whose gout has been quiescent for years with <6 serum urate <6.8 mg/dL would not be incentivized to change urate management just for the purpose of lowering serum urate to less than 6 mg/dL if the patient was clinically doing well.
3. Monitor sUA levels for all gout patients: Consistent tracking of gout patients’ sUA level at specific stages of their care ensures a standardized approach to optimal treatment, Dr. FitzGerald says. According to the eQCMs, if a patient with gout starts or changes urate-lowering therapy, then serum urate should be measured no later than six months after the change. For all patients with gout receiving urate-lowering therapy, serum urate should be measured at least once every 12 months.
4. Understand the value of patient education for optimal, uninterrupted urate-lowering treatment: In general, gout is a poorly managed condition for several reasons, Dr. FitzGerald says. One reason is that gout often gets triaged after other chronic health conditions, such as diabetes, hypercholesterolemia, cardiovascular disease or hypertension. A second reason: Optimal gout management is dependent on adherence to taking medications. But when gout symptoms are quiescent, a patient may choose to stop taking medications, not realizing they are hindering their treatment.3
“Taking time to speak with patients about the importance of taking the drugs supports patient buy-in,” he says. “Applying these quality measures in practice gives rheumatologists and colleagues, including nurses and pharmacists, a way to improve their performance in having these conversations with patients in a consistent way.”
5. Find a way to apply the measures: Of the 10 eCQMs developed by the ACR-supported group, four were endorsed by the ACR’s Quality Measures Subcommittee and two were endorsed by the National Quality Forum. Three measures—evaluating indications for urate-lowering therapy, monitoring serum urate and treat-to-target outcome—were incorporated into the ACR’s Rheumatology Informatics System for Effectiveness (RISE) registry.
“I’m a big fan of RISE because it gives physician practice groups a way to apply quality measures to evaluate their own performance,” Dr. FitzGerald says. He notes that having these data can lead to valuable quality improvement interventions.
Example: UCLA has applied these measures, which resulted in an established process in which a pharmacist within Dr. FitzGerald’s practice checks in with patients to determine that they are taking their gout medication and getting their sUA level checked.
“These measures address the important factors that can make the difference in reaching the outcomes we should all be helping our patients achieve,” Dr. FitzGerald says.
Carina Stanton is a freelance science writer in Denver.
References
- Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the U.S. general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011 Oct;63(10):3136–3141.
- FitzGerald JD, Mikuls TR, Neogi T, et al. Development of the American College of Rheumatology electronic clinical quality measures for gout. Arthritis Care Res (Hoboken). 2018 May;70(5):659–671.
- Aung T, Myung G, FitzGerald JD. Treatment approaches and adherence to urate-lowering therapy for patients with gout. Patient Prefer Adherence. 2017 Apr 19;11:795–800. eCollection 2017.


