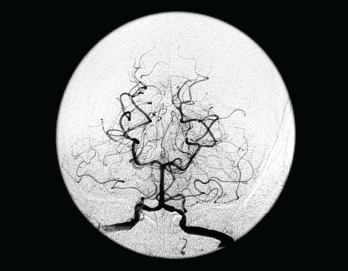
This frontal view from a vertebral angiogram shows the typical appearance of intracranial vasculitis.
Living Art Enterprises, LLC / Science Source
Many a rheumatology consult has centered on a perplexing question: Does this patient have central nervous system (CNS) vasculitis? At the 2021 ACR State-of-the-Art Clinical Symposium, Rula Hajj-Ali, MD, FACP, professor of medicine and associate director of vasculitis care and research, Cleveland Clinic Lerner College of Medicine, discussed this topic in detail, providing a series of clinical pearls that can be helpful in answering this query.
CNS vasculitis can be a primary process or secondary to an underlying condition. Although this entity is rare and diagnosis is often inferential, given the relative inaccessibility of CNS tissue for biopsy, many forms of the condition are treatable if detected early. Dr. Hajj-Ali noted CNS vasculitis can be seen in the context of systemic vasculitides, such as granulomatosis with polyangiitis (GPA), eosiniophilic granulomatosis with polyangiitis (EGPA), Behçet’s disease, giant cell arteritis and Takayasu arteritis. CNS vasculitis can also be associated with such conditions as common variable immunodeficiency (CVID) and a newly recognized genetic disease, deficiency of enzyme adenosine deaminase 2 (DADA2).
Dr. Hajj-Ali indicated the prevalence of CNS involvement in systemic vasculitis is generally low, with 7–11% of patients with GPA and 1–8% of patients with eosinophilic GPA demonstrating such involvement. CNS vasculitis is even rarer in patients with such conditions as systemic lupus erythematosus, Sjögren’s syndrome or sarcoidosis. Yet these scenarios are possible and should be differentiated from primary angiitis of the central nervous system (PACNS).
PACNS: In 1998, Calabrese and Mallek first proposed diagnostic criteria for PACNS, which include: 1) a neurologic deficit that is unexplained after a thorough evaluation, 2) high-probability angiogram for vasculitis or biopsy evidence of vasculitis within the CNS and 3) exclusion of all conditions capable of producing secondary arteritis or mimicking the angiographic features of arteritis.1
In addition to these conditions, potential mimics of PACNS include embolic phenomena from subacute bacterial endocarditis; myxoma and hypercoagulable conditions; infections, such as HIV, hepatitis, varicella zoster virus or neuroborreliosis; and miscellaneous conditions, such as CNS lymphoma, autoimmune encephalitis and demyelinating disorders.
Clinical Pearls
Dr. Hajj-Ali presented seven key insights regarding the diagnostic approach to possible CNS vasculitis.
1. No specific clinical finding or set of findings is sufficient to secure a diagnosis of CNS vasculitis. Rather, pre-test probabilities for this condition must be carefully evaluated in each case.
In a retrospective study of 101 patients with PACNS by Salvarani et al. , headache, altered cognition and hemiparesis were the three most common clinical characteristics. Additionally, mortality rate and disability were greatest in patients with focal neurologic deficits, cognitive impairment, cerebral infarctions and angiographic evidence of large-vessel involvement.2 Thus, the presence of such clinical characteristics does not mean PACNS is definitively confirmed, but the condition can at least be considered as part of the differential diagnosis.
2. Consider lumbar puncture an essential part of the workup for PACNS, unless there is an absolute contraindication, such as mass effect from a possible tumor or other intracranial mass. Not only can cerebrospinal fluid evaluation help rule out other entities, but Salvarani et al. noted cerebrospinal fluid analysis showed one or more abnormal findings in 88% of patients with PACNS. Changes in the cerebrospinal fluid typically included a mild increase in the leukocyte count, total protein concentration or both.2 Although abnormal cerebrospinal fluid findings are generally mild in PACNS, the absence of any abnormalities would argue against the diagnosis.
3. Non-vascular imaging is highly sensitive and has a high negative predictive value for helping rule out PACNS. Example: Diffusion-weighted imaging is a method that creates tissue contrast secondary to water diffusion. This technique can be used in magnetic resonance imaging (MRI) to study the brain and identify pathology that would otherwise go undetected on conventional MRI. White et al. demonstrated that, compared with healthy controls, the apparent diffusion coefficient was significantly increased in patients with CNS vasculitis—even in patients with apparently normal brain imaging on conventional MRI.3
4. There is no angiographic study with 100% specificity for CNS vasculitis. The list of conditions associated with abnormal cerebral angiography include fibromuscular dysplasia, Moyamoya disease, radiation vasculopathy, angiotropic and intravascular lymphoproliferative disorders, and reversible cerebral vasoconstriction syndrome (RCVS).
RCVS is of particular interest because it can be seen in the context of pregnancy or the puerperium period with exposure to certain drugs, such as amphetamines, cocaine, triptans and ergotamine, as well as with conditions, including hypercalcemia, porphyria and pheochromocytoma. Compared with PACNS, RCVS is much more common in women and is associated with thunderclap, rather than insidious, headache. Patients with RCVS also have normal cerebrospinal fluid studies, and an MRI of the brain is normal in up to one-fifth of cases.
5. Brain biopsy is underused as a valuable, albeit imperfect tool. Brain biopsy can help rule in PACNS, given its high positive predictive value and high specificity, and may help rule out mimics in up to 40% of cases. Dr. Hajj-Ali noted that a truly positive biopsy for vasculitis should show transmural inflammation, as well as vascular wall damage. It was also noted that findings of perivasculitis should not be considered equivalent to vasculitis, because infection, hypoxia, trauma and other types of injury can cause perivasculitis.
6. The next piece of advice was that clinicians must rule out infection and cancer in any case of suspected CNS vasculitis. To illustrate this point, Dr. Hajj-Ali presented two clinical cases. In the first, a patient with suspected PACNS based on clinical history, abnormal cerebrospinal fluid and pathology demonstrating granulomatous, angiocentric inflammation with giant cells was ultimately found to have cerebrospinal fluid cultures positive for Mycobacterium tuberculosis. Given the slow-growing nature of this organism, the cultures did not return positive until three weeks after they were collected.
In the second case, a young man with focal neurologic deficits had an MRI showing a subacute cerebellar peduncle infarct. Months later, he had a different subacute cerebellar infarct, and cerebral angiography concerning for vasculitis was ultimately positive for Aspergillus galactomannan in his cerebrospinal fluid. This result returned after he had been treated with corticosteroids, but had an increasing cerebrospinal fluid leukocyte count despite this therapy.
7. In this vein, the final tip from Dr. Hajj-Ali was that when a patient with suspected PACNS does not respond to corticosteroids or cyclophosphamide, it suggests an alternative diagnosis rather than refractory disease.

