Artur Szczybylo / shutterstock.com
In 2005, a workforce study conducted by the ACR projected a shortage of 2,500 rheumatologists by 2025.1 This resulted in an increase in the number of rheumatology fellows trained and the development of online training programs for nurse practitioners and physician assistants in rheumatology.
In 2014, Daniel Battafarano, DO, MACP, was a member of the ACR’s Rheumatology Training & Workforce Issues Committee, which recognized that nearly a decade had passed since the initial workforce study. He and colleagues led a new and comprehensive workforce study that was published in the April 2018 issue of Arthritis Care & Research.2 It had a number of goals: to identify demographic employment trends, assess patient access to care and look for potential solutions to address or account for shortages.
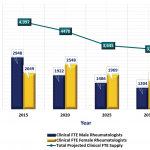
Unfortunately, the new study shows the situation is not improving. By 2025, it projects a shortage of 3,269 rheumatology professionals (physicians, nurse practitioners and physician assistants). By 2030, demand is expected to outpace supply by 102%—the study predicts a shortage of more than 4,000 rheumatology providers.
“It’s an OMG for rheumatologists, and an OMG reality check for most medicine and surgery,” says Dr. Battafarano, professor of medicine at the Uniformed Services University of the Health Sciences and rheumatology fellowship program director at San Antonio Military Medical Center. “The U.S. is not ready for this in 2025.”
The study found wide discrepancies in the availability of rheumatology professionals in each state, with more rheumatologists concentrated in urban and suburban areas of the U.S. while rural areas suffer significant gaps (what Dr. Battafarano and the study refer to as a “geographic maldistribution”).

Dr. Battafarano
“Patients will have trouble getting access to rheumatologists” by 2025, Dr. Battafarano says. This is true across the board, but especially in the Central U.S., the Southwest, Southeast and Northwest, based on a provider distribution rate per 100,000 patients.
“In the Northeast, it looks pretty good right now (with about three rheumatologists per 100,000 patients). [There’s] a density of medical and training programs, and a lot of rheumatologists are training there and staying there,” says Dr. Battafarano, noting that the current acceptable rate is roughly 1.60 providers per 100,000. “What’s undeniable is that by 2025, the rates will be terrible everywhere.”
The updated workforce study also took a deep dive into the shifting demographics of the rheumatology workforce, which Dr. Battafarano sees as representative of most of medicine, although this was not tested in the study.
The study predicts a shortage of more than 4,000 rheumatology providers [by 2030]. ‘It’s an … OMG reality check.’ —Dr. Battafarano
“Looking at the rheumatology workforce is a reflection of the American workforce,” he explains. “We have retiring baby boomers being replaced by a millennial workforce that is leapfrogging gen-Xers, because they outnumber them, … it’s happening in corporate America and it’s happening in healthcare.”