It’s a disorder that can be reliably diagnosed and treated by nonspecialists as part of primary healthcare. Specialist care is needed for a small proportion of individuals with complicated depression or those who do not respond to first-line treatments. The earlier the treatment begins, the more effective it is.

In addition to mood, anhedona and cognition, depression also affects neurovegetative functions, leading to changes in eating and sleeping patterns, with affected individuals doing too much or too little. Individuals with depression report constant fatigue and often “look” depressed, with a slouched posture, unkempt appearance and slowed movements. These somatic complaints are an underappreciated symptom of depression.
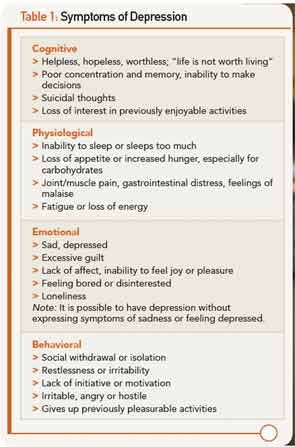
Overlapping symptoms of physical and psychiatric symptoms in co-occurring conditions can create significant barriers to diagnosis. In fact, more than 90% of clients with depression manifest physical symptoms, including muscle or headaches, weakness, gastrointestinal problems, faintness or dizziness, or sensory impairments. Pain occurs frequently with depression, and there is a corollation between the severity of the depression and the severity of the pain.10 Table 1 summarizes the symptoms of major depressive disorder (MDD). The diagnostic focus of these symptoms typically turns to the diagnosis of the physical symptoms without considering depression.
The Need for Appropriate Screening
Care providers are likely to see many clients with undiagnosed depression who come for treatment, and appropriate screenings can lead to a diagnosis and effective intervention. Further, many people with depression “self-medicate” with drugs or alcohol, which exacerbates the effects of depression and worsens overall health. Use of a well-designed screening tool is a valuable adjunct to the information typically gathered during a physician visit.11 However, many patients may present in ways that are atypical or present barriers to recognition.
Older adults with depression present with physical symptoms more than feeling sad or depressed. Fatigue, insomnia, loss of appetite and pain are frequently reported, as well as feeling in “low” spirits.12 Depression negatively affects activity levels, memory, cognition and problem solving, which are also problems frequently seen in older adults.13 In addition, they are more likely to be uncomfortable talking about their sadness and under-report their symptoms. The onset of depression appears to be a significant factor leading to nursing home placement and suicide, further increasing the burden of illness that older adults experience.14 Some care providers mistakenly believe these symptoms are a “normal” part of aging, and too often attribute them to an inevitable component of aging. Conversely, the overlap of symptoms that occur with aging and those that occur with depression may lead to the over-diagnosis of depression.15