Most notable for professionals working with patients with arthritic conditions is the fact that higher levels of depression are associated with increased levels of pain, fatigue, physical distress, levels of disability, worse outcomes following knee replacement, poorer overall health and greater use of healthcare resources.8,9,15 Generally, the more severe the depression, the greater the number and intensity of physical symptoms, which are accompanied by significant restriction of life activities.10 Typically, arthritic patients with depression will present to their care providers with physical symptoms that are seen in both arthritis and depression. As noted above, each of these conditions increases both the symptoms and disease burden of the co-occuring conditions, including joint pain, loss of energy, poor sleep, poor appetite and fatigue. Healthcare providers who treat patients with arthritis must be aware of the impact of this comorbidity and consider depression screening for all patients, but most especially for those patients whose arthritis symptoms increase in severity.
Effectiveness of Screening Tools
The gold standard for diagnosing depression is a structured, or semi-structured, interview by a mental health professional. However, this is neither feasible nor necessary. Multiple screening tools are available that can be easily administered in medical settings. Efficacious tools need to have both good sensitivity and specificity. Sensitivity will rule in, or yield, an accurate number of patients with the condition being screened. Test specificity, on the other hand, will rule out or exclude patients who do not have the target condition without identifying too many false negatives. A concern with test specificity is that too many affected individuals will be missed. Test sensitivity and specificity that are close to 1 are desirable, and .8 is considered good. A test with a sensitivity of .8 will capture 80% of patients who have the disorder being screened for. A specificity of .8 will rule out 80% of patients without the target condition.21
Prevalence rates on these tools will be affected by the threshold for a positive screen that can be raised or lowered to suit the preferences of the examiner. Patients who screen positive for depression will need to be followed up with a structured or semi-structured interview to determine its actual presence.
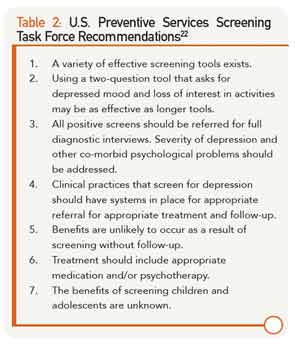
The U.S. Preventive Services Task Force (USPSTF) has developed recommendations for depression screening in medical settings.22 They found there is ample evidence that depression screening improves the identification of depression in primary care settings and improves outcomes for patients. A summary of their recommendations is found in Table 2. All positive screens should be referred for a follow-up diagnostic interview. The best outcomes have resulted when the depression results are communicated with patients and other relevant professionals to facilitate effective intervention and follow-up. Screenings in isolation from intervention and follow-up do not improve outcomes.