The ACR position statement on access to care proposes the goal that “… all patients have timely access to expert rheumatology care … .”1 The reality is that new and established rheumatology patient wait times are often prolonged, causing delays in necessary diagnosis and treatment. The 2005 and 2015 ACR Workforce studies document intractable and worsening shortages of rheumatologists in the U.S., and they propose more fellowships, as well as the hiring and training of advanced practice clinicians (APCs) as physician substitutes.2,3 Improving the productivity of the existing rheumatology workforce has received insufficient attention, in our opinion.
The ACR position statement on access to care proposes the goal that “… all patients have timely access to expert rheumatology care … .”1 The reality is that new and established rheumatology patient wait times are often prolonged, causing delays in necessary diagnosis and treatment. The 2005 and 2015 ACR Workforce studies document intractable and worsening shortages of rheumatologists in the U.S., and they propose more fellowships, as well as the hiring and training of advanced practice clinicians (APCs) as physician substitutes.2,3 Improving the productivity of the existing rheumatology workforce has received insufficient attention, in our opinion.
The Rheumatoid Arthritis Practice Performance (RAPP) project was an industry-supported clinical process improvement project conducted by 170 participating community rheumatologists between 2013 and 2015 to overcome barriers to providing treat-to-target care of rheumatoid arthritis (RA) patients. The methods, findings and initial impacts of their practice changes on access to care, disease activity assessments and disease control have been presented in multiple forums.4-6
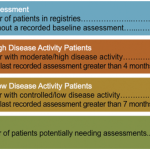
RAPP project participants identified their traditional, physician-centric, visit-based care as the universal bottleneck that limited access for new and existing patients and for effective management during these visits. As we previously reported, they were able to resolve this bottleneck by implementing team care and standardized population medicine processes that increased their per physician panel sizes and reduced their per patient costs of care.
This article describes the longer-term experiences of three RAPP practices drawn from the majority that have also achieved sustained improvements in their access, care and financial performance. They include a solo practice; a multi-physician, single-specialty practice; and a large, multi-specialty group practice. The implications are compelling for broadly resolving the rheumatology workforce shortage and practice productivity problems that plague our specialty and the patients who require our care.
Long-Term Practice Improvement
Practice No. 1: William Arnold, MD, & Erin Arnold MD, Skokie, Ill.
Orthopaedics and Rheumatology of the North Shore (ORNS), S.C., is a small partnership practice founded in 2014 by Drs. William (Bill) and Erin Arnold, father and daughter, merging with a father–son orthopedic surgery practice. Their participation in the first 2013 RAPP consultants’ meeting enabled Drs. Bill and Erin Arnold to successfully plan for his 2016 retirement, and for Dr. Erin Arnold to continue in solo practice. She continues to employ two medical assistants and an ultrasound technician, and has since added one physician assistant to her staff.
Fundamental practice changes have allowed Dr. Erin Arnold to absorb her father’s patients and then further grow her patient panel. These include separating the assessment and management components of patient visits, and standardizing disease assessments to include a Routine Assessment of Patient Index Data 3 (RAPID3) with a review of systems, swollen joint count, Vectra test, and a technician-performed, standardized ultrasound exam at predefined intervals. All team members participate in assessments and documentation to reduce Dr. Erin Arnold’s established patient workload, while she focuses on four new patient consultations per day and established patients with problems.