The ACR position statement on access to care proposes the goal that “… all patients have timely access to expert rheumatology care … .”1 The reality is that new and established rheumatology patient wait times are often prolonged, causing delays in necessary diagnosis and treatment. The 2005 and 2015 ACR Workforce studies document intractable and worsening shortages of rheumatologists in the U.S., and they propose more fellowships, as well as the hiring and training of advanced practice clinicians (APCs) as physician substitutes.2,3 Improving the productivity of the existing rheumatology workforce has received insufficient attention, in our opinion.
The ACR position statement on access to care proposes the goal that “… all patients have timely access to expert rheumatology care … .”1 The reality is that new and established rheumatology patient wait times are often prolonged, causing delays in necessary diagnosis and treatment. The 2005 and 2015 ACR Workforce studies document intractable and worsening shortages of rheumatologists in the U.S., and they propose more fellowships, as well as the hiring and training of advanced practice clinicians (APCs) as physician substitutes.2,3 Improving the productivity of the existing rheumatology workforce has received insufficient attention, in our opinion.
The Rheumatoid Arthritis Practice Performance (RAPP) project was an industry-supported clinical process improvement project conducted by 170 participating community rheumatologists between 2013 and 2015 to overcome barriers to providing treat-to-target care of rheumatoid arthritis (RA) patients. The methods, findings and initial impacts of their practice changes on access to care, disease activity assessments and disease control have been presented in multiple forums.4-6
RAPP project participants identified their traditional, physician-centric, visit-based care as the universal bottleneck that limited access for new and existing patients and for effective management during these visits. As we previously reported, they were able to resolve this bottleneck by implementing team care and standardized population medicine processes that increased their per physician panel sizes and reduced their per patient costs of care.
This article describes the longer-term experiences of three RAPP practices drawn from the majority that have also achieved sustained improvements in their access, care and financial performance. They include a solo practice; a multi-physician, single-specialty practice; and a large, multi-specialty group practice. The implications are compelling for broadly resolving the rheumatology workforce shortage and practice productivity problems that plague our specialty and the patients who require our care.
Long-Term Practice Improvement
Practice No. 1: William Arnold, MD, & Erin Arnold MD, Skokie, Ill.
Orthopaedics and Rheumatology of the North Shore (ORNS), S.C., is a small partnership practice founded in 2014 by Drs. William (Bill) and Erin Arnold, father and daughter, merging with a father–son orthopedic surgery practice. Their participation in the first 2013 RAPP consultants’ meeting enabled Drs. Bill and Erin Arnold to successfully plan for his 2016 retirement, and for Dr. Erin Arnold to continue in solo practice. She continues to employ two medical assistants and an ultrasound technician, and has since added one physician assistant to her staff.
Fundamental practice changes have allowed Dr. Erin Arnold to absorb her father’s patients and then further grow her patient panel. These include separating the assessment and management components of patient visits, and standardizing disease assessments to include a Routine Assessment of Patient Index Data 3 (RAPID3) with a review of systems, swollen joint count, Vectra test, and a technician-performed, standardized ultrasound exam at predefined intervals. All team members participate in assessments and documentation to reduce Dr. Erin Arnold’s established patient workload, while she focuses on four new patient consultations per day and established patients with problems.
High-performing practices use clinical process improvement methods to effectively manage their disease populations with robust care teams.
Dr. Erin Arnold limits her new patients to those with probable rheumatic diseases. Her wait times are less than two weeks, and she saw 662 new patients in 2018. Her schedule has increased from 24 to 33 patients per day (33%). Over five years, the ORNS RA patient population has increased from 700, when Dr. Bill Arnold retired, to 1,700. The total number of patient visits in 2016 and 2019 numbered 6,399 and 8,931 respectively. This increased productivity has more than paid for increased staffing. Dr. Erin Arnold is able to successfully balance her professional and family time, while her father enjoys his retirement and his daughter’s success.
This increased capacity has not compromised the practice’s quality of care or patient satisfaction. The Arnolds’ baseline disease activity distributions were among the most favorable in the RAPP project. These have improved further even as Dr. Erin Arnold has continued to add new, active RA patients (see Table 1).
Table 1: Vectra Test RA Disease Activity Distribution (%)
| 2014 | 2019 | |
|---|---|---|
| Controlled/Low | 38 | 56 |
| Moderate | 37 | 31 |
| High | 25 | 13 |
Practice No. 2: Gary Crump, MD, Louisville, Ky.
Rheumatology Associates PLLC is an independent rheumatology practice with three physicians and four nurse practitioners. It cares for patients from the Greater Louisville, Ky., area. The practice maintains an in-office infusion center and an imaging facility that offers digital X-ray and technician-performed musculoskeletal ultrasound. Laboratory testing is provided by a commercial laboratory and several specialty reference labs.
When Dr. Crump participated in the first 2013 RAPP project consultants meeting, he was a junior partner in a five-physician practice that employed no APCs. Each rheumatologist cared for their separate, relatively small patient panels and used paper records. After two partners left the practice, Dr. Crump bought out his senior partner, and the other stayed on as an employee. He has since employed one additional rheumatologist and another is on deck. Unlike his previous partners, Dr. Crump’s new colleagues are like-minded about team care and continuous practice improvement, because he assessed these characteristics before hiring them. A partnership option is available.
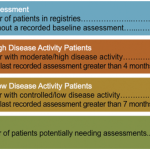
The practice has also added four APCs who work collaboratively with the physicians. The APCs see the majority of established RA patients for assessment and routine management visits. The practice uses standardized assessments, including RAPID3 and the Clinical Disease Activity Index (CDAI), at every visit. Vectra tests and diagnostic ultrasounds with scoring protocols are added at specified frequencies based on a patient’s disease activity status. The care team has developed and copyrighted rheumatic disease care pathways to further facilitate team care. Staff proactively track missed appointments and other services for all patients. The analytic electronic medical record (EMR) provides individual and population run charts based on standardized clinical metrics. Encounter documentation formats have been standardized and recently upgraded voice recognition software has been implemented.
Dr. Crump’s practice has dramatically improved its access and productivity from 2013 to 2018. Its RA population has increased from 122 to 521 patients per physician. New patient visits per year per physician have increased from 468 to 832. New patient wait times have decreased from six to four weeks, on average. The practice’s current RA population’s Vectra test distribution is 51% controlled, 24% moderate and 25% high disease activity.
Physician and staff satisfaction and camaraderie are high, and the practice has low employee turnover. Rheumatology Associates honors patients’ preferences for physician and APC visits, and surveys reflect a high level of patient satisfaction. Dr. Crump has shortened his work week to four days while increasing his productivity, allowing him to pursue his passion for riding and driving American Saddlebred horses.
Practice No. 3: David Sikes, MD, Zephyrhills, Fla.
Florida Medical Clinic (FMC) is an independent, physician-owned multi-specialty group founded in 1993 by Dr. Sikes, a gastroenterologist and family physician in an underserved rural area near Tampa, Fla. In 25 years, FMC has grown to 275 physicians and 75 APCs, representing most medical and surgical specialties. It now cares for 1.6 million citizens in two counties, including Northeast Tampa and the adjoining rural area. It owns 14 campuses, with a robust complement of laboratories, medical imaging centers, a cardiac catheterization center, physical therapy services, infusion centers and clinical research programs. The center purchased the Greenway EMR in 1995, and continues to redesign it to support the center’s clinical and business needs. The administration continues to be physician led.
When Dr. Sikes attended the first 2014 RAPP project consultant meeting, his rheumatology department included three physicians practicing traditionally with only one APC—a PharmD. The RAPP project motivated him to transform the practice’s staffing, clinical processes, patient access and quality of care. It has standardized and expanded disease activity and other clinical assessments, including training APCs to perform joint examinations. Practice performance measures have been established, and these data are being used to guide patient management and other improvement projects.
In six years, the center has added two rheumatologists, five nurse practitioners/physician assistants, three infusion nurses, a pharmacy technician and three ultrasound technicians, building a comprehensive interdisciplinary care team using disease population medicine processes. The diagnostic ultrasound and infusion services are expanded product lines. Everyone works to the top of their license (i.e., practicing to the full extent of their education and training) to perform total patient work and free the physicians to do what only they can do for many more patients.
Depending on the individual patient’s disease activity, comorbidities and complexity, an office visit may involve different combinations of physicians and staff. Pre-visits are used to obtain ultrasound and lab testing in advance. One unique innovation involves the PharmD, a pharmacy technician, two patient counselors and the medical assistants, who coordinate all patients’ medication prescriptions, education and pre-certifications.
The growth of Dr. Sikes’ rheumatology department and his own practice has been driven not only by the transition from physician-centric to team practice, but also by the increase in patients managed by Florida Medical Clinic overall, the broadening of his department’s scope of practice to provide comprehensive musculoskeletal disease care, and more rigorous and timely APC patient assessment visits.
Between 2013 and 2018, the center maintained a four-week wait time for routine new patient visits in spite of 110% growth in total new patient referrals per year, while also implementing a 48-hour priority scheduling process.
About 20% of established patients are managed for RA, similar to other large multi-specialty group rheumatology practices, but lower than many single specialty practices that focus more on inflammatory rheumatic diseases. Team care has enabled Dr. Sikes’ personal RA panel to grow by 25%, even as he spends one day each week in group administration. His RA population’s disease activity distribution has improved over time, as with other practices that have implemented more robust, on-time assessment processes (see Table 2).
Table 2: Vectra Test RA Disease Activity Distribution (%)
| 2014 | 2015 | 2019 | |
|---|---|---|---|
| Controlled/Low | 18 | 17 | 34 |
| Moderate | 43 | 37 | 45 |
| High | 39 | 46 | 20 |
The growth and success of FMC and its rheumatology practice have derived from the culture of innovation in practice and patient service instilled by Dr. Sikes and his founding colleagues from the outset. FMC has carefully chosen new physicians who share this perspective.
Visitors comment on the rheumatology team’s joy in working together. Patient feedback reflects appreciation for the efficiency, predictability, thoroughness and accessibility of their care.
While Dr. Sikes maintains a busy practice and administrative schedule, he finds time for family, training for competitive bicycle team racing and regular ballroom dancing with his spouse.
Implications
These examples of rheumatology practice transformation in very different clinical environments are typical of how exceptional medical specialty practices manage all chronic diseases, as was described in a 2012 book, Great Health Care: Making It Happen.7 High-performing practices use clinical process improvement methods to effectively manage their disease populations with robust care teams. The 2012 examples informed the RAPP project, and we hope these successes will inform broader improvement across rheumatology and the other medical specialties, because within practices, no matter what diseases are involved, it is how care is delivered and managed that makes all the difference.
The RAPP Project physicians identified nine steps for transforming rheumatology practices that we hope our colleagues will implement. Step 9 on the list below may be the first you need to take:
- Define your scope of practice and acceptable wait times, and then modify your scheduling and new patient appointment processes to align with your intentions;
- Track all patients’ disease activity by adopting a bundle of measures and standardized assessment intervals, and then treat to target;
- Build a practice team to free your schedule for the work that only you can do. This includes adding APCs to manage established patients’ disease assessments, reconcile their treatments, coordinate their care, complete required record documentation, provide patient education and review their findings with you. This physician-APC collaborative approach is fundamentally different from, and more successful than, APCs serving as physician substitutes. It can also be implemented rapidly;
- Focus your own work on managing more new consultations and sicker established patients. More new patients will rapidly grow your managed patient population and revenues without compromising access to your personal care when needed. Patients understand and approve of this;
- Use simple analytic disease registries to identify your disease population, to track patients’ disease activity status and to coordinate their management;
- Track your practice’s visit volumes, wait times, disease outcomes and financial performance with defined measures and simple analytic information technology to document and continuously improve your performance;
- As your managed patient population grows, expand your team to manage more patients per physician at a lower per patient cost before adding more rheumatologists. Then invite like-minded colleagues to join your high-performing practice;
- Focus on restoring joy to your own and your team members’ professional and personal lives; but
- If your present practice environment won’t allow you to make these improvements, consider moving and/or retaking control of the patient care you provide.
Our new book, Great Health Care Value guides practices in how to manage these changes, rapidly and with minimal disruptions to existing patient care, based on what we learned from the RAPP project.6
Conclusion
Dr. Bill Arnold observed, “The problems rheumatologists face are ours to solve because how we deliver care is the primary problem.”
These problems can be solved if, and only if, we improve our productivity by providing care for many more patients per physician, on time and at a lower per patient cost. The RAPP project documents that this is realistic—and our only realistic solution. We can make this happen.
The affiliations of Drs. Erin and William Arnold, Gary Crump and David Sikes are within the article. Andrew Johnson is the principal of PopMed Solutions LLC, Washington, D.C., and Dr. Timothy Harrington was the principal of Harrington Consulting LLC, prior to his death in June 2020.
Editor’s note: See p. 21 in this issue for Dr. Harrington’s obituary.
References
- American College of Rheumatology. Position statement. Access to care. 2019 Sep.
- Deal CL, Hooker R, Harrington T, et al. The United States rheumatology workforce: Supply and demand, 2005–2025. Arthritis Rheum. 2007 Mar;56(3):722–729.
- Academy for Academic Leadership. 2015 Workforce Study of Rheumatology Specialists in the United States. Atlanta. 2016.
- Arnold E, Arnold W, Conaway D, et al. Rheumatoid Arthritis Practice Performance project spots problems in RA management. The Rheumatologist. 2015 Jun;9(6):44–46.
- Harrington T, Arnold E, Arnold W, et al. Help wanted: The rheumatology workforce shortage revisited. The Rheumatologist. 2016 May;10(5):38–39,53.
- Harrington T, Johnson A. Great Health Care Value: Chronic Diseases, Practice Teams, and Population Management. Madison, Wis.: Self-published, 2019.
- Great Health Care: Making It Happen. JT Harrington JT, Newman ED (eds.). New York: Springer, 2011.