Implications
These examples of rheumatology practice transformation in very different clinical environments are typical of how exceptional medical specialty practices manage all chronic diseases, as was described in a 2012 book, Great Health Care: Making It Happen.7 High-performing practices use clinical process improvement methods to effectively manage their disease populations with robust care teams. The 2012 examples informed the RAPP project, and we hope these successes will inform broader improvement across rheumatology and the other medical specialties, because within practices, no matter what diseases are involved, it is how care is delivered and managed that makes all the difference.
The RAPP Project physicians identified nine steps for transforming rheumatology practices that we hope our colleagues will implement. Step 9 on the list below may be the first you need to take:
- Define your scope of practice and acceptable wait times, and then modify your scheduling and new patient appointment processes to align with your intentions;
- Track all patients’ disease activity by adopting a bundle of measures and standardized assessment intervals, and then treat to target;
- Build a practice team to free your schedule for the work that only you can do. This includes adding APCs to manage established patients’ disease assessments, reconcile their treatments, coordinate their care, complete required record documentation, provide patient education and review their findings with you. This physician-APC collaborative approach is fundamentally different from, and more successful than, APCs serving as physician substitutes. It can also be implemented rapidly;
- Focus your own work on managing more new consultations and sicker established patients. More new patients will rapidly grow your managed patient population and revenues without compromising access to your personal care when needed. Patients understand and approve of this;
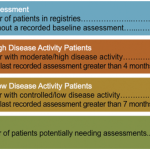
- Use simple analytic disease registries to identify your disease population, to track patients’ disease activity status and to coordinate their management;
- Track your practice’s visit volumes, wait times, disease outcomes and financial performance with defined measures and simple analytic information technology to document and continuously improve your performance;
- As your managed patient population grows, expand your team to manage more patients per physician at a lower per patient cost before adding more rheumatologists. Then invite like-minded colleagues to join your high-performing practice;
- Focus on restoring joy to your own and your team members’ professional and personal lives; but
- If your present practice environment won’t allow you to make these improvements, consider moving and/or retaking control of the patient care you provide.
Our new book, Great Health Care Value guides practices in how to manage these changes, rapidly and with minimal disruptions to existing patient care, based on what we learned from the RAPP project.6