Simone Hogan / shutterstock.com
At the 2021 ACR State-of-the-Art Clinical Symposium, Saira Sheikh, MD, associate professor of Medicine and director of the Rheumatology Lupus Clinic, University of North Carolina, Chapel Hill, provided an update on the past, present and future of the management of systemic lupus erythematosus (SLE).
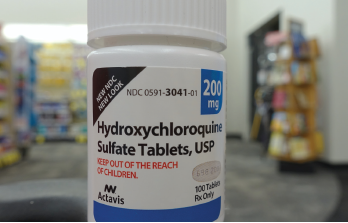
This year, hydroxychloroquine received a great deal of attention, given early reports that it might be beneficial in the prevention and treatment of COVID-19. Clinical trials did not support this hypothesis, and the medication is not recommended for COVID-19 treatment. In fact, the U.S. Food & Drug Administration (FDA) issued a statement in June 2020 warning that co-administration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended, because it reduces the anti-viral activity of remdesivir.1
Hydroxychloroquine remains a mainstay of lupus treatment and is recommended for all patients with SLE, unless a specific contraindication exists. It’s possible to assess hydroxychloroquine adherence using drug levels in the blood, but insufficient data presently exist to recommend such monitoring in routine clinical practice.
Dr. Sheikh noted the recommended daily dose of hydroxychloroquine is 5 mg/kg of body weight. Additionally, screening for retinopathy with visual field examination and/or spectral domain-optical coherence tomography should be performed at baseline and annually after five years of use.
Treatment Goals
Although Dr. Sheikh remarked that patients with SLE often describe intangible symptoms, such as fatigue, brain fog and depression, which require further research to understand and treat, an overarching goal in the management of SLE should be a treat-to-target approach. In this regard, the concepts of remission of disease and lupus low disease activity state (LLDAS) can be employed.
In Dr. Sheikh’s presentation, remission indicates the absence of disease activity and steroid use in patients with SLE who are being managed with hydroxychloroquine alone. For LLDAS, this goal indicates an SLE Disease Activity Index 2000 (SLEDAI-2K) score of less than 4, with no activity from major organ systems; a Physician Global Assessment of less than 1, with no new activity; a prednisone dose of less than 7.5 mg daily; and standard doses of antimalarials, immunosuppressives and biologics.
How can clinicians achieve these goals? For lupus nephritis, Dr. Sheikh indicated that at least three years of treatment, including one year of complete clinical remission, should be achieved before considering withdrawal of immunosuppression.
When such withdrawal occurs, the potential risks include increased disease activity and flares, worse renal outcomes, and increased morbidity and mortality.
Complicating the matter is that, often, a discrepancy exists between clinical and histologic responses to treatment, with 30% of patients categorized as complete responders demonstrating histologic evidence of activity on renal biopsy, which is strongly predictive of a subsequent renal flare when reducing immunosuppression.
Treatment Advances
On a positive note, two medications have recently been approved by the FDA for the treatment of lupus nephritis: belimumab and voclosporin.
Belimumab is a fully humanized IgG1γ monoclonal antibody directed against soluble B lymphocyte stimulator (BLyS). In the BLISS-LN study, 448 patients with biopsy-proven, active lupus nephritis were randomized to receive 10 mg/kg of intravenous belimumab or matching placebo in addition to standard therapy (i.e., either induction with high-dose steroids and intravenous cyclophosphamide using the Euro-Lupus protocol, and maintenance with low-dose steroids and 2 mg/kg of azathioprine per day; or induction with high-dose steroids and mycophenolate mofetil 3 g/day and maintenance with low-dose steroids and mycophenolate mofetil 1–3 g/day). The primary endpoint at week 104 was a primary efficacy renal response, defined as a ratio of urinary protein to creatinine of less than 0.7, an estimated glomerular filtration rate of no worse than 20% below the pre-flare value or greater than 60 mL/minute/1.73 m2 of body-surface area and no use of rescue therapy. 3
In the study, 43% of belimumab-treated patients achieved the primary endpoint, compared with 32% of placebo-treated patients. The risk of a renal-related event or death was lower among patients who received belimumab than among those who received placebo, with a hazard ratio of 0.51.3 Given these data, belimumab may be a useful adjunctive therapy when added to standard care for treating lupus nephritis.
In the AURORA 3 study, 357 patients with active lupus nephritis were randomized to receive the calcineurin inhibitor voclosporin at a dose of 23.7 mg twice per day or placebo in combination with 2 g per day of mycophenolate mofetil and rapidly tapered oral steroids. Patients could receive intravenous methylprednisolone up to 1 g on day 1 and 2, with tapering of oral corticosteroids to 2.5 mg per day by week 16. The study’s primary endpoint was renal response at 52 weeks, defined as urine protein to creatinine ratio of less than 0.5 mg/mg, estimated glomerular filtration rate (eGFR) greater than 60 mL/min or no confirmed decrease from baseline in eGFR of greater than 20%, presence of sustained, low-dose steroids and no administration of rescue medication.4
In this trial, 40.8% of voclosporin-treated patients achieved the primary endpoint vs. 22.5% of placebo-treated patients. Proteinuria reduction in the voclosporin group was twice as fast compared with standard of care alone, and the group receiving voclosporin demonstrated significantly greater renal response vs. controls as early as week 24.4
Thus, voclosporin in addition to mycophenolate mofetil appears to be helpful to treat patients with lupus nephritis. Of particular interest, ethnicity subgroup analysis in the AURORA 3 study indicates voclosporin is effective in Hispanic/Latino patients, a group that has traditionally had difficult to treat disease. This finding, coupled with the lower toxicity and side effect profile of voclosporin vs. the older calcineurin inhibitors, such as cyclosporine and tacrolimus, make this medication a potentially appealing option in many clinical scenarios.
Dr. Sheikh ended her presentation with several thought-provoking questions: Could belimumab and voclosporin become part of the standard of care to treat lupus nephritis? What is the role of cyclophosphamide in the treatment of patients with SLE in the modern era? What parameters, such as adherence, pregnancy considerations and renal function, should guide the selection of medications in the treatment of each patient with SLE?
As this lecture clearly demonstrated, the future of lupus management is both complex and exciting, and the rheumatology community will have to ask these and other important questions while seeking to help patients in the years ahead.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- U.S. Food & Drug Administration. Medical product safety information: Remdesivir by Gilead Sciences: FDA warns of newly discovered potential drug interaction that may reduce effectiveness of treatment. 2020 Jun 15.
- Tselios K, Gladman DD, Urowitz MB. How can we define low disease activity in systemic lupus erythematosus? Semin Arthritis Rheum. 2019 Jun;48(6):1035–1040.
- Furie R, Rovin BH, Houssiau F, et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med. 2020 Sep 17;383(12):1117–1128.
- Arriens C, Polyakova S, Adzerikho I, et al. AURORA phase 3 study demonstrates voclosporin statistical superiority over standard of care in lupus nephritis (oral presentation: OP0277). Ann Rheum Dis. 2020;79:172–173.


