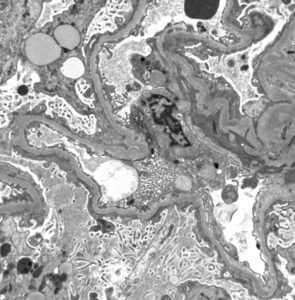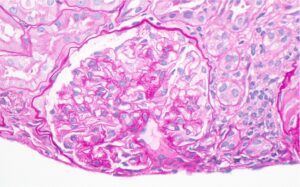
Figure 1: Hematoxylin and eosin (H&E) stain with normal appearing glomeruli or with the minimal change. (Click to enlarge.)
Kidney involvement is a major cause of morbidity and mortality in systemic lupus erythematosus (SLE). Collectively termed lupus nephritis, SLE with kidney involvement comes in many subtypes. The current classification by the International Society of Nephrology/Renal Pathology Society (ISN/RPS), however, does not include lupus podocytopathy, which, through various clinical and epidemiologic studies, has recently been recognized as a distinct subtype of lupus nephritis.1
Lupus podocytopathy is defined clinically as nephrotic-range proteinuria and histology showing normal glomeruli or only mild glomerular mesangial proliferation.2 Studies have shown that 0.6–1.5% of all lupus nephritis biopsies reveal lupus podocytopathy.1,3
In 2002, Dube et al. and Hertig et al. described 18 patients with SLE and nephrotic syndrome with renal biopsy showing minimal change disease (MCD) or focal segmental glomerulosclerosis (FSGS) changes.4,5 Later, in 2016, Hu et al. described 50 patients with lupus podocytopathy with improved understanding of the condition as a distinct entity.2 One of the characteristic features of lupus podocytopathy is responsiveness to glucocorticoid therapy. Despite the growing awareness of lupus podocytopathy, high-quality data on the disease course and management of lupus podocytopathy is lacking, particularly in cases of treatment resistance. We present a case of glucocorticoid refractory lupuspodocytopathy with relapse.
Case Presentation
A 70-year-old woman with SLE presented with generalized edema and fatigue for two weeks, associated with exertional shortness of breath and foamy urine. Manifestations of her SLE included inflammatory arthritis and leukopenia; her antinuclear antibody (ANA) titer was positive at 1:320, along with antidouble-stranded DNA (dsDNA) positivity (46 IU/mL; normal <9 IU/mL) and SSA positivity (8 AI [autobody index]; normal <0.9 AI). She had been treated with 5 mg/kg of hydroxychloroquine monotherapy for the past three years.
Her physical examination was remarkable for severe generalized edema. Laboratory data revealed anemia, with hemoglobin of 9.2 g/dL (normal range 11.7–15.5 g/dL); leukopenia, with white cell count of 1.52 k/uL (normal 3.8–10.8 k/uL); elevated creatinine at 2.5 mg/dL above her baseline of 0.65 mg/dL; estimated glomerular filtration rate (eGFR) of 24 mL/min/1.73 m2; elevated erythrocyte sedimentation rate (ESR) 69 mm/hr (normal <20 mm/hr); and hypoalbuminemia of 0.9 g/dL (normal 3.6–5.1 g/dL). Urinalysis showed hematuria (red blood cell [RBC] count of >180/high power field [HPF]) and nephrotic range proteinuria, with a urine protein to creatinine ratio (UPCR) of 12,888 mg/g.