After the first dose of rituximab, the patient was noted to have a stable renal response, with an eGFR of 44 mL/min/1.73 m2, creatinine of 1.30 mg/dL and urine protein to creatinine ratio of 469 mg/g.
Discussion
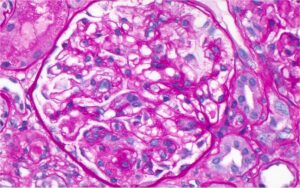
Lupus podocytopathy clinically presents as nephrotic range proteinuria, which correlates with the extent of foot process effacement.3,6 The diagnostic criteria proposed by Hu et al. are:2
- Clinical presentation: nephrotic range proteinuria, hypoalbuminemia and edema; and
- Histologic picture:
- minimal change disease (MCD), mesangial proliferative change or focal segmental glomerulosclerosis (FSGS); immunofluorescence showing minimal immunoglobulin and complement deposition or no immune complex deposition in mesangial areas; and absence of subepithelial and subendothelial immune complex deposition;
- presence of diffuse podocyte foot process effacement (FPE) on electron microscopy, typically >70%.
Additionally, features of endocapillary proliferation, crescents and necrosis are absent in lupus podocytopathy.3 Podocyte injury by other causes, such as thrombotic microangiopathy, should be excluded.3,7 Our patient met the above clinical and histological criteria for lupus podocytopathy.
Based on histopathology, lupus podocytopathy can be divided into three subtypes: 1) MCD (normal light microscopy without mesangial proliferation); 2) FSGS; and 3) mesangioproliferative lupus nephritis (class 1 or 2 lupus nephritis changes with podocytopathy).1 The mesangial form is the most common form of lupus podocytopathy.1 The FSGS subtype is associated with acute kidney injury and tubulointerstitial involvement, and is further classified as not otherwise specified (NOS), perihilar, cellular, tip or collapsing variant, of which the collapsing variant has the worst prognosis.1,3,8
Although the pathogenesis of lupus podocytopathy is not well understood, direct podocyte injury mediated by cytokines, lymphokines or T cell dysfunction, rather than immune complex deposition is thought to be the driving force.3,9,10 In general, lupus podocytopathy is considered a glucocorticoid-responsive entity. Following the Kidney Disease Improving Global Outcome (KDIGO) treatment guidelines for MCD, lupus podocytopathy can be treated with 1 mg/kg of glucocorticoids, tapered over six months after achieving complete remission (defined as reduction of proteinuria to <0.3 g/day, stable serum creatinine and serum albumin of >3.5 g/dL) or based on clinical response.11,12
A high risk of relapse has been reported with glucocorticoid monotherapy.2 In Hu et al.’s study, there were no differences in response for induction with glucocorticoids alone vs. glucocorticoids with immunosuppression. But more than half the patients with lupus podocytopathy who were on maintenance with glucocorticoids alone relapsed.2