BALTIMORE—The eye may be the window to the soul, but in medicine it can also serve as a harbinger of systemic disease. At the 18th Annual Advances in the Diagnosis and Treatment of the Rheumatic Diseases, held May 13–14 at the Johns Hopkins School of Medicine, Baltimore, Meghan Berkenstock, MD, associate professor of ophthalmology, Wilmer Eye Institute, Johns Hopkins School of Medicine, gave a presentation on the connection between rheumatology and ophthalmology.
BALTIMORE—The eye may be the window to the soul, but in medicine it can also serve as a harbinger of systemic disease. At the 18th Annual Advances in the Diagnosis and Treatment of the Rheumatic Diseases, held May 13–14 at the Johns Hopkins School of Medicine, Baltimore, Meghan Berkenstock, MD, associate professor of ophthalmology, Wilmer Eye Institute, Johns Hopkins School of Medicine, gave a presentation on the connection between rheumatology and ophthalmology.
Dr. Berkenstock discussed three main topics: 1) the association of uveitis with systemic disease, 2) medications and vaccinations that can be associated with the development of uveitis, and 3) when it’s appropriate to refer patients to an ophthalmologist.
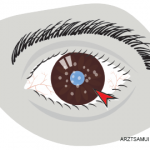
Uveitis is an umbrella term for intraocular inflammation that can apply to more than 30 different syndromes, Dr. Berkenstock explained. The etiologies of uveitis can be autoimmune, infectious, neoplastic or idiopathic, and one or more chambers of the eye can be affected. Inflammation of the eye is a rare phenomenon because the eye is generally an immune-privileged site.
Rheumatic Disease
In rheumatoid arthritis (RA) and secondary Sjögren’s syndrome associated with keratoconjunctivitis sicca, patients may experience eye dryness, foreign-body sensation, photophobia and red eyes. An increased risk for external infections exists secondary to decreased tear turnover and breakdown of surface epithelium, which can lead to painful and recurrent filamentary keratitis.
Treatments for dry eye associated with Sjögren’s syndrome include artificial tears, punctal plugs, topical cyclosporine or tacrolimus, lifitegrast, oral pilocarpine, scleral lenses and autologous serum tears. One of the newest treatments approved by the U.S. Food & Drug Administration for the management of dry eyes is varenicline nasal spray, which may be helpful for select patients.
Patients with RA can also develop scleritis or episcleritis, Dr. Berkenstock explained. If a patient develops scleritis associated with peripheral corneal melting (i.e., peripheral ulcerative keratitis), it’s particularly important to evaluate for the possibility of underlying RA. For episcleritis in RA, this condition is typically self-limited but can recur, and treatment may involve topical glucocorticoids and topical non-steroidal anti-inflammatory drugs (NSAIDs).
In patients with scleritis, it’s important to evaluate for conditions beyond RA, such as HLA-B27-associated spondyloarthritis, Lyme disease, anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis and sarcoidosis. The treatment of scleritis typically begins with oral non-steroidal anti-inflammatory drugs (NSAIDs) and can escalate to systemic glucocorticoids—up to the equivalent of 1 mg/kg of prednisone daily. If inflammation recurs before tapering to 7.5 mg or less of prednisone daily, then methotrexate, mycophenolate mofetil or tumor necrosis factor-α (TNF) inhibitors, should be considered.
Dr. Berkenstock noted that if scleral perforation or extensive thinning exists and there is a high risk of scleral rupture, surgery may be necessary.
Acute Anterior Uveitis
In ankylosing spondylitis, a strong association with both HLA-B27 positivity and acute anterior uveitis exists. This form of uveitis can recur or become chronic, may present bilaterally or alternate between eyes, and can occur simultaneously with scleritis. The classic presentation of acute anterior uveitis is eye redness, pain, blurred vision and photophobia.
Screening for Lyme disease, sarcoidosis and syphilis in these patients is important, according to Dr. Berkenstock. Also, RA and systemic lupus erythematosus can, rarely, present with acute anterior uveitis. Treatment of this condition includes topical glucocorticoids; posterior sub-tenon injection with triamcinolone acetonide or other medication; and, in cases of chronic anterior uveitis or in patients who do not tolerate local therapy, oral glucocorticoids and immunomodulators may be appropriate.
The prognosis for these patients tends to be good, with the average episode lasting six weeks or less. However, complications, such as cataracts, macular edema, glaucoma, corneal decompensation, hypotony or phthisis, may occur.
In sarcoidosis, the eye is one of the most commonly affected organs, & ocular manifestations include granulomatous uveitis, inflammatory glaucoma, optic neuropathy or granulomatous infiltration, & more.
Sarcoidosis
In sarcoidosis, the eye is one of the most commonly affected organs, and ocular manifestations can include granulomatous uveitis, inflammatory glaucoma, optic neuropathy or granulomatous infiltration, and lacrimal gland enlargement with sicca syndrome.
In granulomatous uveitis, the patient may present with mutton fat precipitates on the corneal endothelium. This condition usually involves both eyes in a progressive fashion. Patients may also demonstrate periphlebitis, which is common in the peripheral retina, with perivascular sheathing and severe vasculitis associated with extensive perivascular exudates. Patients whose eyes are subject to these changes may experience venous occlusion and neovascularization.
In patients with granulomatous inflammation of the optic nerve, the optic disc may have a characteristic lumpy and white appearance. Fortunately, recovery of vision for patients with granulomatous inflammation of the optic nerve can be rapid and significant if corticosteroids are started in a timely manner. These patients should also undergo neuroimaging to evaluate central nervous system involvement.
Medications Linked to Uveitis
Medications associated with uveitis include TNF inhibitors, bisphosphonates, oral contraceptives, sildenafil, sulfas, rifabutin, quinidine and clomiphene. Fluoroquinolones may also be associated with uveitis.
Various vaccines have also been associated with the development of uveitis, including those for influenza, hepatitis B, measles/mumps/rubella (MMR), diphtheria/pertussis/tetanus (DPT), varicella and the bacille Calmette-Guerin (BCG) vaccine for tuberculosis. Although more data are needed, reports also exist of patients presenting with uveitis after vaccination against COVID-19.1
Referrals
With respect to referral to ophthalmology, Dr. Berkenstock noted that ocular immunology specialists see patients with a range of conditions, including Behçet’s disease, relapsing polychondritis, systemic vasculitis, multiple sclerosis, temporal arteritis and central nervous system lymphoma. Certainly, in patients with a red, painful eye and a recent infection, particularly syphilis, tuberculosis, varicella zoster, toxocara or toxoplasmosis, expert eye care may be highly beneficial.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
Reference
- Ferrand N, Accorinti M, Agarwal M, et al. COVID-19 vaccination and uveitis: Epidemiology, clinical features and visual prognosis. Ocul Immunol Inflamm. 2022 Apr 11;1–9.